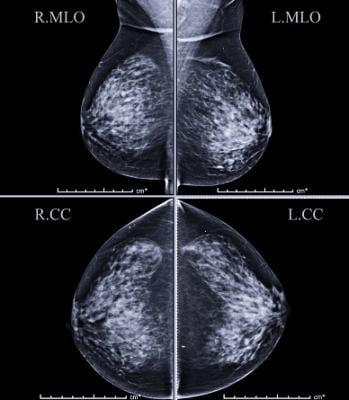
Getty Images
May 19, 2020 — Women with mammographically detected breast lesions that are probably benign should have follow-up surveillance imaging at six months due to the small but not insignificant risk that the lesions are malignant, according to a new study published in the journal Radiology.
The Breast Imaging and Reporting System (BI-RADS) was established by the American College of Radiology to help classify findings on mammography. Findings are classified based on the risk of breast cancer, with a BI-RADS 2 lesion being benign, or not cancerous, and BI-RADS 6 representing a lesion that is biopsy-proven to be malignant.
BI-RADS 3, a probably benign finding, is a particularly challenging category that can cause confusion for physicians and anxiety for patients. This assessment means that the lesion is one of a few specific findings that has been shown to have less than a 2 percent chance of being cancer and that any cancer present is not likely to spread in the time frame recommended for follow-up imaging.
The interval for follow-up imaging has been a point of contention in the breast imaging community. Some earlier research suggested that malignancies were so rare in the BI-RADS 3 group that follow-up could be safely pushed back from six months to a year. However, much of that research was done before the advent of the National Mammography Database (NMD).
“I thought that we should really look at this again now that we’ve got this large database we can work with and try to find out what happened with these patients,” said study lead author Wendie A. Berg, M.D., Ph.D., a renowned breast cancer researcher at the University of Pittsburgh School of Medicine and professor of radiology at UPMC Magee-Womens Hospital in Pittsburgh.
Berg and colleagues assessed outcomes from six-, 12-, and 24-month follow-up of probably benign findings first identified on recall from screening mammography in the NMD. The study group included women recalled from screening mammography with BI-RADS 3 assessment at additional evaluation over a period of almost 10 years. The women in the study group had no personal history of breast cancer and underwent either biopsy or two-year imaging follow-up.
Out of 43,628 women given BI-RADS 3 assessment after screening mammography recall, 810 (1.9%) were diagnosed with cancer. About a third had ductal carcinoma in situ (DCIS), an early-stage, noninvasive form of breast cancer. However, 12% of the invasive cancers diagnosed within six months with node staging had spread to the lymph nodes.
“The majority of cancers were diagnosed at or right after the six-month follow-up, so it actually is important to get these patients back in that six-month time frame,” Berg said.
The malignancy rates in the BI-RADS 3 group substantially exceeded those of women downgraded to BI-RADS 1 or 2 at each follow-up, further supporting short-interval follow-up imaging surveillance.
“The important thing about this paper is that these data come from a wide number of facilities across the United States, so it really brings to bear that, yes, this is the appropriate practice and yes, you still need to see these patients in six months,” Berg said.
Berg has also been studying how a personal history of breast cancer affects malignancy rates in women with BI-RADS 3 findings. Preliminary findings she reported at the 2019 RSNA annual meeting indicate that the malignancy rate could be as high as 15%.
“That suggests that we should probably be much more cautious about BI-RADS 3 findings in those patients,” she said.
For more information: www.rsna.org


 February 05, 2026
February 05, 2026 









