Jan. 26, 2026 — Researchers at the University of Arizona were awarded up to $1.8 million by the Advanced Research Projects Agency for Health, or ARPA-H, an agency within the U.S. Department of Health and Human Services, to develop a lymphatic scanner small and light enough for physicians to bring with them to diagnose and monitor patients with lymphatic disease.
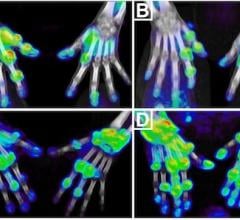
Lymphatic disorders affect hundreds of millions of people worldwide. Standard imaging modalities like lymphoscintigraphy, magnetic resonance and ultrasound fall short in providing sufficient detail for physicians to make reliable diagnoses and proceed with the most effective treatment available. This limitation leads to the misdiagnosis and poor outcomes for many patients with lymphatic-related disorders.
The "Game Changing Quantitative and Targeted Multimodal Lymphatic Imaging to Go" team will use the ARPA-H funds to create a new modality called Phase Change Ultrasound Lymphograph, or PCUS, capable of super-resolution mapping of lymphatic structures. Russell Witte, professor of radiology and imaging sciences at the College of Medicine – Tucson and member of the BIO5 Institute, will lead the team.
"What we are looking to do is to fill an unmet need for better methods of looking at the lymphatic system – having something that's portable, accessible to patients and simple to use," Witte said. "Our goal is to build a device to provide images in real time that can provide quantitative information on the anatomy and function of a person's lymphatic system."
Because lymphatic vessels are tiny, collapsible and translucent, they are much harder to see than blood vessels. Lymph fluid is normally under low pressure and moving very slowly, which makes it much more challenging to track than blood flowing in arteries and veins.
Using phase change contrast agents, the PCUS device will map lymph flow, lymphatic vessels and nodes to screen for lymphatic abnormalities and pinpoint obstruction sites. The information will help medical professionals monitor patients and guide treatment decisions. Witte and the team hope to have the new modality and medical device available for use within the next five years.
"The goal is to make something that is affordable and accessible that reveals how the lymphatic system is actually functioning and malfunctioning," said program manager Dr. Marlys Witte, an international specialist in lymphology, professor of surgery and director of multilevel student research programs at the College of Medicine – Tucson. "With this technology, we are not only going to see it, we are going to see how lymphatics contract and how fast lymph flows. And then if we examine and treat the patient, we will be able to see whether the flow is improving or whether an obstruction is being removed."
The funding comes from ARPA-H's Lymphatic Imaging, Genomics, and pHenotyping Technologies program (LIGHT), led by ARPA-H program manager Dr. Kimberley Steele. The program's overarching goal is to illuminate the unseen aspects of the lymphatic system through imaging technologies, prevention, prediction and diagnostic confirmation, and diagnosis and monitoring through biomarker discovery.
The ARPA-H award is the first of its kind at the University of Arizona. As part of the award, the BIO5 Institute will provide $128,000 in cost sharing to upgrade the Translational Biomedical Imaging Resource Core Facility.
"We hope to help address conditions that are linked to problems with the lymphatic system," Witte said. "The lymphatic system is not well understood, so there's a component of the project to bring awareness to the lymphatic system, as well as to develop new technologies for interfacing with the system."
Causes of lymphatic disorders range from tropical worm infestations to complications of cancer treatment. They are commonly associated with limb swelling, or lymphedema, and other disorders that affect internal organs and cause birth defects and various tumors that extend from head to toe.
Other U of A co-investigators on the team include Terry Matsunaga, research professor in the Department of Neurosurgery at the College of Medicine – Tucson; Lars Furenlid, professor in the Department of Radiology and Imaging Sciences at the College of Medicine – Tucson; Ali Bilgin, associate professor of biomedical engineering at the College of Engineering; and Mitchell Bartlett, associate scientific investigator in the Department of Surgery at the College of Medicine – Tucson.


 March 06, 2026
March 06, 2026