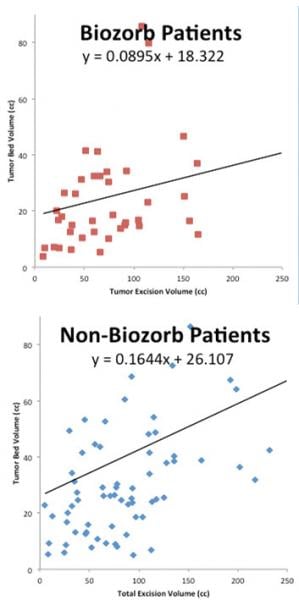
May 30, 2017 — Patients who were implanted with the BioZorb 3-D bioabsorbable marker during their lumpectomy could be treated with smaller radiation volumes than patients who did not receive the marker, according to new research. The findings were presented at the recent American Society of Breast Surgeons (ASBrS) annual meeting, April 26-30 in Las Vegas. The difference in volumes was statistically significant.
A scientific poster by Kara Lynn Leonard, M.D. reported that patients who received the marker were treated with substantially less radiation than patients whose tumors were defined during the treatment planning stage with free clips or no clips.
Leonard concluded that "the BioZorb system may offer an advantage in more precisely defining the lumpectomy site and in sparing larger volumes of healthy breast tissue from radiation." The poster also said the implant is particularly helpful for boost planning.
The study was a retrospective analysis of women who had received radiation treatment for breast cancer in the radiation oncology department at Rhode Island Hospital, in Providence, R.I. The study covered all women treated at the department during the year-long span from May 2015 through April 2016. The data encompassed 117 patients — 42 of whom received a BioZorb implant and 75 who did not.
The researchers compared records of women who received the marker to the records of patients who were not implanted with the device. Most of the women who did not have the marker implanted were treated before the device was adopted for use by the department.
Among measurements recorded for each patient were the amount of tissue removed during each patient's lumpectomy, and the amount of radiation each patient was targeted to receive — that is, the tumor bed volume. The tumor bed volume was substantially smaller for the patients who received the BioZorb device, a difference that was statistically significant.
More accurate radiation has several potential benefits for breast cancer patients. It can help improve cosmetic outcomes as well as help to protect healthy body structures such as the heart and lungs from radiation exposure.
Leonard is a radiation oncologist at Rhode Island Hospital (Providence, R.I.) and an assistant professor of radiation oncology at The Warren Alpert Medical School of Brown University.
BioZorb is the first and only device, according to manufacturer Focal Therapeutics, that identifies in a reliable way the three-dimensional region where the tumor was removed. By suturing the implant to the tumor bed, the surgeon can more precisely indicate to the radiation oncologist where the cancer was located. Because of the marker's unique configuration, it allows oncoplastic surgery to be used for reconstructing the breast with the patient's own tissues, while at the same time delineating the tumor's previous location.
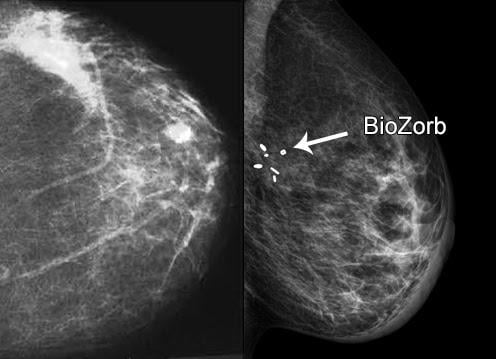
The marker consists of a framework made of a bioabsorbable material that holds six titanium clips. The implant serves as a guide for the radiation oncologist during planning of radiation treatments that are delivered after surgery. The device's framework slowly dissolves in the body over the course of a year or more. The marker clips remain at the surgical site and can be viewed for long-term monitoring. Studies have reported the complication rate such as infection (2-3 percent) is virtually the same as for lumpectomy surgery and follow-up radiation without the implant.
For more information: www.focalrx.com


 February 18, 2026
February 18, 2026 









