October 26, 2020 — Results of a new randomized phase III trial suggest that stereotactic radiosurgery (SRS) should replace whole brain radiation therapy (WBRT) as the standard of care for patients with four or more brain metastases. Compared with whole-brain treatment, highly focused radiation therapy led to less cognitive decline with equivalent overall survival. Results from the clinical trial (NCT01592968) was presented today at the American Society for Radiation Oncology (ASTRO) Annual Meeting.
“This study provides strong evidence to support replacing whole brain radiation with more focal radiation for patients with multiple brain metastases,” said lead author Jing Li, M.D., Ph.D., an associate professor of radiation oncology and co-director of the Brain Metastasis Clinic at The University of Texas MD Anderson Cancer Center in Houston.
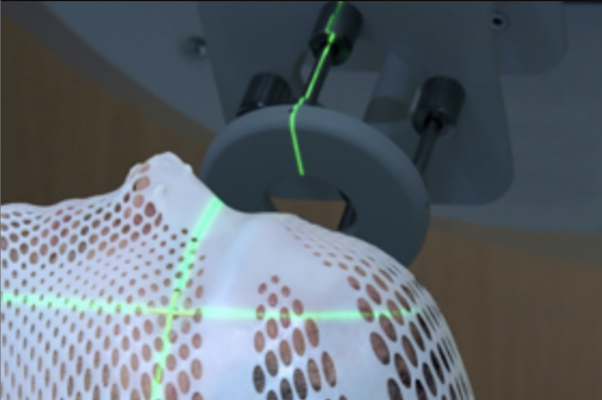
The trial builds on previous research that established SRS as the standard of care for patients with one to three brain metastases. "Whole brain radiation was the backbone of treatment for brain metastases for a very long time. When stereotactic radiosurgery became available, however, we saw its potential to reduce the cognitive deterioration associated with whole-brain treatment and improve patients' quality of life," said Li. SRS is more convenient for patients and minimizes interruption of systemic therapy, as well; while WBRT typically is given in 10 treatment sessions over a period of two weeks, radiosurgery generally is completed in one single-day session.
An estimated 1 in 5 patients with cancer will develop brain metastases when primary cancers, most commonly breast cancer, lung cancer or melanoma, spread to the brain. Brain metastases are diagnosed in an estimated 150,000-200,000 people each year, with rising incidence as improved treatments help patients live longer.
In this randomized phase III trial, radiation oncologists at MD Anderson treated 72 adult patients who had 4-15 untreated, non-melanoma brain metastases with either SRS (n=36) or WBRT (n=36). Patients in the WBRT arm were also recommended memantine, a prescription drug used to treat dementia, after a different phase III trial found that it helped delay cognitive decline in patients receiving WBRT for brain metastases. Researchers tracked cognitive function through standard tests of learning and memory, attention span, executive function, verbal fluency, processing speed and motor dexterity.
Cognitive function was better preserved for patients who received SRS, compared to those who received WBRT. Four months after radiation therapy, patients in the SRS group scored higher on a memory function test than they did at baseline (average z-score change from patient’s own baseline, +0.21). Patients in the WBRT group arm scored worse on the memory function test compared to baseline (average z-score change, -0.74; p=0.04). Four months after treatment, 6% of the patients in the SRS arm experienced a clinically meaningful decline in cognitive function, compared to 50% of patients in the WBRT arm (p=0.018).
"Cognitive decline is one of the most debilitating effects of brain metastases and treatment, and a key goal of treatment is to improve functioning in the brain for patients with these tumors," explained Li. Previous trials have indicated that upwards of 90% of patients with brain metastases experience cognitive impairment before treatment, most commonly trouble with attention, memory or information processing.
Overall survival did not differ between the groups (SRS median 7.8 months, WBRT median 8.9 months, p=0.59). Local control rates favored SRS, but the difference did not reach statistical significance (95% at four months with SRS and 86.7% with WBRT (p=0.09). The median time to distant brain failure was 10.5 months for WBRT and 6.3 months for SRS (p=0.37).
Radiosurgery, compared to WBRT, was associated with shorter interruptions of systemic therapy (time to systemic therapy: SRS 1.7 weeks, WBRT 4.1 weeks, p=0.001). This finding is particularly important for patients with metastatic disease, explained Dr. Li, as they benefit from systemic therapy to control cancer outside of the brain.
Four patients who received WBRT (15%) and two who received SRS developed (8%) grade 3 or higher toxicities. Radiographic evidence of radiation necrosis, a side effect associated with SRS, was observed in 17% patients on the SRS arm of the trial (4% of all treated lesions).
Next steps for the research team include comparing SRS with a newer form of WBRT designed specifically to avoid the hippocampus, a brain structure that is central to learning and memory. While a recently published trial (NRG Oncology CC 001) found an advantage of hippocampal-avoidance over standard whole-brain treatment, no trial has compared it with SRS. "Both options are currently considered standard treatment, and both options have pros and cons. We need randomized data to understand which patients will benefit most from each of these treatments," said Dr. Li.
For more information: www.astro.org


 February 04, 2026
February 04, 2026 









