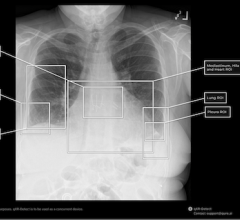
Dice similarity index—comparison of x-ray pulsatility index to digital subtraction angiography. XPI (green), pulmonary angiography (pink), overlap (white)
May 17, 2024 — The Cum Laude Award-Winning Online Poster presented during the 124th ARRS Annual Meeting found that the noncontrast x-ray pulsatility index (XPI) method to evaluate and monitor pulmonary blood flow could improve clinical efficiency as a screening or diagnostic test, provide substantial financial benefits, and improve patient satisfaction.
“Additionally,” said Matthew Smith, MD, from Vanderbilt University Medical Center in Nashville, TN, “this easy-to-implement method can be performed by an x-ray technologist in an outpatient setting,”
Smith et al. enrolled volunteers suspected of chronic thromboembolic pulmonary hypertension (CTEPH) based on pulmonary scintigraphy and/or CTA. Fluoroscopic acquisition (70 kV, 30 frames/s) over an 8-second breath hold was performed in either RAO (30°) or LAO (40°) for the right and left lung, respectively. The temporal signal from each pixel was decomposed into individual frequency components via Fourier transform. The researchers then isolated heart rate signal oscillation using a band-pass filter and amplitude XPI mapped to form an image. Immediately following each fluoroscopic acquisition for spectral analysis, digital subtraction pulmonary angiography was performed with catheter-injected contrast in the same projection using standard protocols. Perfusion maps were segmented using a blinded manual technique, as well as a semi-automated threshold and region-growing method, while segmentation maps were compared using the Dice similarity coefficient—a statistical measurement of overlap.
Ultimately, in this ARRS Annual Meeting Cum Laude Scientific Poster, where noncontrast (XPI) and contrast pulmonary angiography images were obtained in 11 different lungs, all patients were able to perform satisfactory breath hold, despite moderate to severe disease. Direct comparison of segmentation maps revealed an average Dice score of 0.77, suggesting excellent agreement between XPI and pulmonary angiography maps in depicting regions of blood flow and, more importantly, lack of blood flow.
For more information: www.arrs.org


 March 06, 2026
March 06, 2026