
September 24, 2015 — The Jumpstarting Brain Tumor Drug Development Coalition (JBTDDC) announced a new consensus protocol for magnetic resonance imaging (MRI) in brain tumor clinical trials to help better assess if a new treatment is effective. The coalition’s Brain Tumor Imaging Standardization Steering Committee published its recommended new standards for acquisition of imaging data in multicenter clinical trials, called the Brain Tumor Imaging Protocol (BTIP), in the advanced access online edition of the journal Neuro-Oncology.
The development and adoption of a standardized MRI protocol in brain tumor clinical trials will help validate and build confidence in the use of quantitative imaging surrogates as endpoints for drugs seeking U.S. Food and Drug Administration (FDA) approval, including but not limited to the ‘Accelerated Approval’ pathway. In addition, a standardized protocol will incentivize brain tumor drug development by providing an accepted way to capture imaging information essential to the evaluation of future treatments.
“Malignant brain tumors, particularly glioblastomas, are some of the most complex and treatment-resistant cancers,” said Mark Gilbert, M.D., chair of the Brain Tumor Imaging Standardization Steering Committee and chief of the Neuro-Oncology Branch of the National Cancer Institute. “Glioblastoma patients have a median survival of only 14-16 months, and fewer than 10 percent survive beyond five years of their diagnosis. With limited treatment options available, there is a critical need to quickly identify new, effective therapies for this patient population.”
As is the case across all oncology clinical trials, Overall Survival (OS) is the “gold standard” measurement of investigational brain tumor therapies’ effectiveness. However, OS trials are lengthy and expensive. Therefore, the field of neuro-oncology has a long-standing interest in using alternative endpoints that use imaging to measure tumor progression and response to determine the relative value of an investigational treatment.
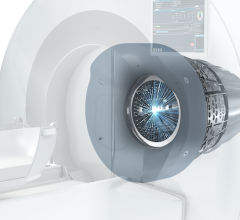
Traditionally, response and progression are measured in neuro-oncology using MR imaging. However, there have been issues with variability in the interpretation of images and tumor measurements between observers and between treatment centers. The lack of standards in MR imaging acquisition protocols and differences in MR scanners (i.e. field strength, gradient system, manufacturer sequences) has limited the ability to combine imaging data across sites in a multicenter clinical trial study.
“It is well known that even minor differences in hardware or sequence timing may result in significant changes in image contrast,” said Benjamin Ellingson, Ph.D., of the Department of Radiological Sciences at the David Geffen School of Medicine at UCLA, and lead author of the BTIP paper. “Moreover, a variety of MR protocols are commonly used for the same purpose, further hindering interpretation of imaging results from different treatment centers in the absence of tight control and standardization of image acquisition parameters.”
The Brain Tumor Imaging Steering Committee published the new BTIP with scientific and practical justifications for the recommendations. The protocol is designed to minimize patient burden and has taken into account the different capabilities of imaging instruments across international medical centers. In addition, it incorporates new features that allow for potential enhancements in the analysis of tumor imaging data.
The next phase of this effort is to achieve field-wide clinical trial adoption and use of the protocol. The JBTDDC is actively requesting from major U.S. and European neuro-oncology clinical trial co-operative groups, as well as biopharmaceutical sponsors, the incorporation of the protocol as the standard for use in their future brain tumor clinical trials.
For more information: www.braintumor.org

 March 09, 2026
March 09, 2026 









