May 2, 2019 — A new position statement from interventional radiology professional societies in the U.S. and Europe states that prostatic artery embolization (PAE) is a safe, effective and minimally invasive treatment for enlarged prostate, and should be presented as a treatment option for appropriately selected patients. The position statement was authored by the Society of Interventional Radiology (SIR), the Cardiovascular and Interventional Radiological Society of Europe (CIRSE), the Société Française de Radiologie (SFR) and the British Society of Interventional Radiology (BSIR).
The multisociety and multidisciplinary position statement, which was published in the May edition of SIR’s Journal of Vascular and Interventional Radiology,1 recommends PAE as a “valuable minimally invasive option for patients who cannot tolerate or who have failed medical therapy, and those who are poor surgical candidates or refuse invasive surgery.”
Enlarged prostate, also known as benign prostatic hyperplasia (BPH), is one of the most common medical conditions in older men, affecting 70 percent of men over 70. More than 20 studies including more than 2,000 patients with moderate to severe lower urinary tract symptoms (LUTS) due to BPH show that PAE has shorter recovery and fewer complications than traditional surgery and improves symptoms and quality of life to a greater degree than medical therapy.
The societies endorse PAE as “a definitive treatment option for multiple underserved patient groups, who may not have satisfactory urologic treatment options.” These patient groups include older patients with multiple medical conditions, patients with very large prostates, patients with bleeding from the prostate, patients with long-term bladder catheters, patients who cannot stop anti-coagulation therapies and patients who desire to preserve sexual function. “These patients are often poor candidates for surgery, but can be excellent candidates for PAE,” the societies said in the statement.
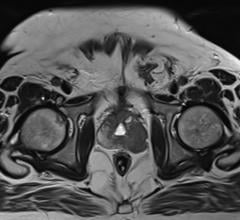
During PAE, an interventional radiologist makes a tiny puncture in either the groin or wrist to insert a catheter into an artery and, using image guidance, directs the catheter to the blood vessels on both sides of the enlarged prostate gland. The doctor uses small beads to block the blood flow to the prostate, which results in the gland’s shrinkage. Unlike surgery, PAE avoids access through the urethra, anesthesia and hospitalization.
In addition to the four societies that authored the guidelines, the guidelines were endorsed by the Asia Pacific Society of Cardiovascular and Interventional Radiology, Canadian Association for Interventional Radiology, Chinese College of Interventionalists, Interventional Radiology Society of Australasia, Japanese Society of Interventional Radiology, and Korean Society of Interventional Radiology.
For more information: www.jvir.org
Reference
1. McWilliams J.P., Bilhim T.A., Carnevale F.C., et al. Society of Interventional Radiology Multisociety Consensus Position Statement on Prostatic Artery Embolization for Treatment of Lower Urinary Tract Symptoms Attributed to Benign Prostatic Hyperplasia: From the Society of Interventional Radiology, the Cardiovascular and Interventional Radiological Society of Europe, Société Française de Radiologie, and the British Society of Interventional Radiology. Journal of Vascular and Interventional Radiology, published online March 26, 2019. DOI: https://doi.org/10.1016/j.jvir.2019.02.013


 July 25, 2024
July 25, 2024