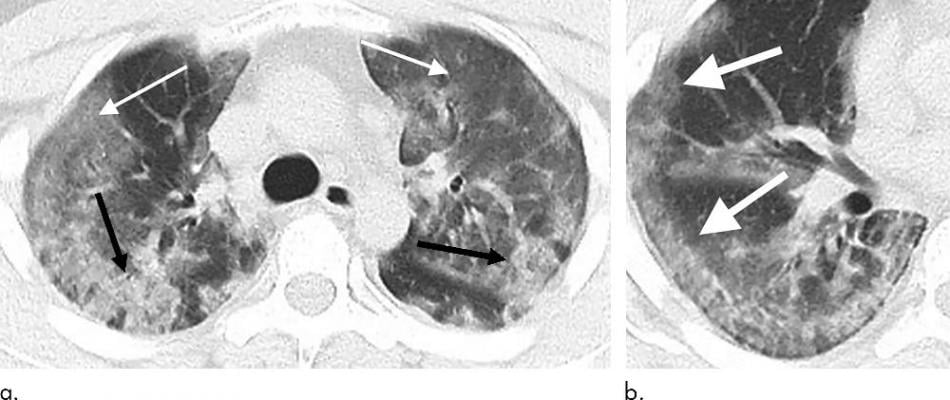
29-year old male with unknown exposure history, presenting with fever and cough, ultimately requiring intensive care unit admission. (a) Axial thin-section non-contrast CT scan shows diffuse bilateral confluent and patchy ground-glass (solid arrows) and consolidative (dashed arrows) pulmonary opacities. (b) The disease in the right middle and lower lobes has a striking peripheral distribution (arrow). Image courtesy of Radiology
February 26, 2020 — Mount Sinai Health System physicians—the first experts in the country to analyze chest computed tomography (CT) scans of patients from China with coronavirus disease (COVID-19)—have identified specific patterns in the lungs as markers of the disease as it develops over the course of a week and a half. The finding, published in the February issue of Radiology, could lead to quicker diagnosis in patients who come in with possible COVID-19 symptoms, and help keep patients isolated in early stages when the lung disease may not show up in initial scans.
“This work augments our initial study, which was the first published research study on the imaging findings of COVID-19, and now we are able to provide a more comprehensive evaluation of how lung disease in coronavirus patients manifests and develops. If coronavirus should continue to spread and impact the United States or elsewhere more significantly, this study equips radiologists with the knowledge to recognize and more confidently suggest if a patient has COVID-19 or pneumonia due to another cause,” said co-author Michael Chung, M.D., assistant professor of diagnostic, molecular and interventional radiology at the Icahn School of Medicine at Mount Sinai. “This is necessary for prompt diagnosis for any individual patient (which will lead to more rapid and effective care), but also for patient isolation to prevent the spreading of the highly contagious disease.”
The study encompassed scans of 94 patients that Mount Sinai received from institutional collaborators at hospitals in China. The patients were admitted to four medical centers in four Chinese provinces between January 18 and February 2. Most either had recently traveled to Wuhan, China, where the outbreak began, or had contact with an infected COVID-19 patient. The cardiothoracic radiologists from Mount Sinai’s BioMedical Engineering and Imaging Institute and its Department of Radiology evaluated each case, took notes of imaging findings, and correlated them with infection time course based on the number of days between symptom onset and the CT scan. Of the 36 patients scanned zero to two days after reporting symptoms, more than half showed no evidence of lung disease—an important finding suggesting that CT scans cannot reliably rule out COVID-19 early in the disease course. For the 33 patients scanned three to five days after symptoms developed, radiologists started to see more patterns of “ground glass opacities” (hazy findings in the lungs), and the abnormalities became more round in shape and more dense. In the 25 patients scanned six to 12 days after symptoms, the scans analysis showed fully involved lung disease. Patterns seen in these images are similar to patterns in related coronavirus outbreaks earlier this century, including SARS (severe acute respiratory syndrome) and MERS (Middle East respiratory syndrome).
The conclusions from this study are crucial for prompt diagnosis of COVID-19 as well as for efficient patient isolation. When patients first report symptoms of possible COVID-19, they are nonspecific, often resembling a common cold, so it can be difficult to diagnose. A chest X-ray does not reveal lung disease as well as a CT scan does, and confirmatory tests by the Centers for Disease Control and Prevention can take several days. The study allows hospitals in the United States and worldwide to confirm or rule out COVID-19 based on CT images. Additionally, if lung scans for patients with early symptoms are inconclusive, doctors can consider holding the patient in isolation for a few days until the disease can be properly ruled in or ruled out.
“Just as clinicians are evaluating more patients suspected of COVID-19, radiologists are similarly interpreting more chest CTs in those suspected of infection. Chest CT is a vital component in the diagnostic algorithm for patients with suspected infection, particularly given the limited availability and in some cases reliability of test kits,” said lead author Adam Bernheim, M.D., assistant professor of diagnostic, molecular and interventional radiology at the Icahn School of Medicine at Mount Sinai. “These investigative efforts not only show patterns of imaging findings in a large number of patients, but they also demonstrate that frequency of CT findings is related to disease time course. Recognizing imaging patterns based on infection time course is paramount for not only understanding the disease process and natural history of COVID-19, but also for helping to predict patient progression and potential complication development.”
“Mount Sinai’s imaging programs are leaders in the development and application of novel technologies to improve patients’ diagnosis and treatment, and we hope the findings from this study will help advance care for coronavirus patients,” added Zahi Fayad, Ph.D., director of the BioMedical Imaging and Engineering Institute at the Icahn School of Medicine at Mount Sinai.
For more information: www.mountsinai.org
Related Coronavirus Content:
The Cardiac Implications of Novel Coronavirus
Radiologists Describe Coronavirus CT Imaging Features
Coronavirus Update from the FDA
CT Imaging of the 2019 Novel Coronavirus (2019-nCoV) Pneumonia
Infervision in the Frontlines Against the Coronavirus
CT Imaging Features of 2019 Novel Coronavirus (2019-nCoV)
Chest CT Findings of Patients Infected With Novel Coronavirus 2019-nCoV Pneumonia


 February 04, 2026
February 04, 2026 









