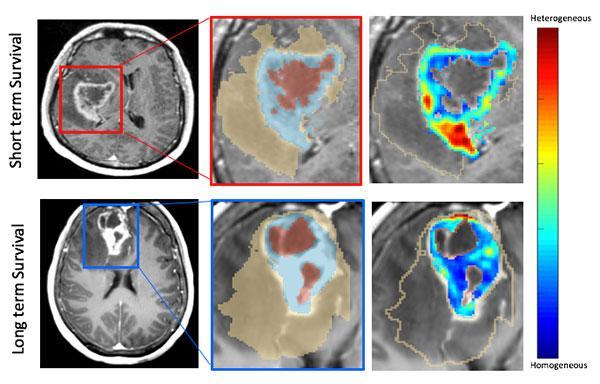
An example of the MRI scans showing long-term and short-term survival indications. Image courtesy of Case Western Reserve University
February 21, 2020 — Glioblastoma is an aggressive, killer disease. While victims of this fast-moving brain tumor comprise only about 15 percent of all people with brain cancer, its victims rarely survive more than a few years after diagnosis.
But research scientists and doctors from the Case Western Reserve University School of Medicine, Case School of Engineering and Cleveland Clinic have blended two very different types of analysis to better understand and combat the brain cancer.
The researchers used the tools of artificial intelligence (AI) — in this case, computer image analysis of the initial magnetic resonance imaging (MRI) scans taken of brain cancer patients — and compared that image analysis with genomic research to analyze the cancer.
The result: A new and more accurate way to not only determine the relative life expectancy of glioblastoma victims--but identify who could be candidates for experimental clinical drug trials, said Pallavi Tiwari, Ph.D., an assistant professor of biomedical engineering at Case Western Reserve with dual appointments in the School of Medicine and Case School of Engineering.
The study was led by Tiwari, along with Niha Beig, a PhD student in Tiwari's lab. Their research was published this month in Clinical Cancer Research, a journal of the American Association for Cancer Research.
Unique study of MRI images, gene expression
The AI model used by the researchers leveraged features from the region adjacent to the tumor, as well as inside the tumor to identify which patients had a poor prognosis, Pallavi said. Then, they used gene-expression information to shed light on which biological pathways were associated with those images.
"Our results demonstrated that image features associated with poor prognosis were also linked with pathways that contribute to chemo-resistance in glioblastoma. This could have huge implications in designing personalized treatment decisions in glioblastoma patients, down the road." she said.
"While we're just at the beginning, this is a big step, and someday it could mean that if you have glioblastoma, you could know whether you'll respond to chemotherapy well or to immunotherapy, based on a patient's image and gene profiles," said Manmeet Ahluwalia, M.D., Miller Family Endowed Chair of NeuroOncology at the Burkhardt Brain Tumor and Neuro-Oncology Center at Cleveland Clinic, and a co-author of the study.
Beig said the researchers were able to compare the MRI scans of patients' tumors with the corresponding genomic information about that same patient, drawn from a National Institutes of Health database.
"That's why this study is unique," she said. "Most researchers look at one or the other, but we looked at both the MRI features and the gene expression in conjunction."
"We can tell you who is at a better risk of survival," Beig said. "What clinicians want to do is give their patient an idea of quality of life, and since roughly 10% of these patients go on to live more than three years, that's important information."
Anant Madabhushi, Ph.D., the F. Alex Nason Professor II of Biomedical Engineering at Case Western Reserve and a co-author on this study, said the research is also important because it "connects the macro features of the tumor to the molecular."
Madabhushi said a common criticism of radiomics--drawing conclusions about tumors from the computer analysis of the images alone--is that the process is opaque and not easily interpretable.
"This is the corroborating evidence," he said. "This shows that molecular changes in the tumor are manifesting as unique representations on the scan."
For more information: https://clincancerres.aacrjournals.org/
To read the original article: Finding New Clues to Brain Cancer Treatment


 February 06, 2026
February 06, 2026 









