The Centers for Medicare & Medicaid Services (CMS) has determined that the evidence is sufficient to add a lung cancer screening, counseling and shared decision making visit, and for appropriate beneficiaries, annual screening for lung cancer with low dose computed tomography (LDCT), as an additional preventive service benefit under the Medicare program only if all of the following criteria are met:
Beneficiary eligibility criteria:
- Age 55 – 77 years;
- Asymptomatic (no signs or symptoms of lung cancer);
- Tobacco smoking history of at least 30 pack-years (one pack-year = smoking one pack per day for one year; 1 pack = 20 cigarettes);
- Current smoker or one who has quit smoking within the last 15 years; and
- Receives a written order for LDCT lung cancer screening that meets the following criteria:
- For the initial LDCT lung cancer screening service: a beneficiary must receive a written order for LDCT lung cancer screening during a lung cancer screening counseling and shared decision making visit, furnished by a physician (as defined in Section 1861(r)(1) of the Social Security Act) or qualified non-physician practitioner (meaning a physician assistant, nurse practitioner, or clinical nurse specialist as defined in §1861(aa)(5) of the Social Security Act). A lung cancer screening counseling and shared decision making visit includes the following elements (and is appropriately documented in the beneficiary’s medical records):
- Determination of beneficiary eligibility including age, absence of signs or symptoms of lung cancer, a specific calculation of cigarette smoking pack-years; and if a former smoker, the number of years since quitting;
- Shared decision making, including the use of one or more decision aids, to include benefits and harms of screening, follow-up diagnostic testing, over-diagnosis, false positive rate, and total radiation exposure;
- Counseling on the importance of adherence to annual lung cancer LDCT screening, impact of comorbidities and ability or willingness to undergo diagnosis and treatment;
- Counseling on the importance of maintaining cigarette smoking abstinence if former smoker; or the importance of smoking cessation if current smoker and, if appropriate, furnishing of information about tobacco cessation interventions; and
- If appropriate, the furnishing of a written order for lung cancer screening with LDCT.
- For subsequent LDCT lung cancer screenings: the beneficiary must receive a written order for LDCT lung cancer screening, which may be furnished during any appropriate visit with a physician (as defined in Section 1861(r)(1) of the Social Security Act) or qualified non-physician practitioner (meaning a physician assistant, nurse practitioner, or clinical nurse specialist as defined in Section 1861(aa)(5) of the Social Security Act). If a physician or qualified non-physician practitioner elects to provide a lung cancer screening counseling and shared decision making visit for subsequent lung cancer screenings with LDCT, the visit must meet the criteria described above for a counseling and shared decision making visit.
- Written orders for both initial and subsequent LDCT lung cancer screenings must contain the following information, which must also be appropriately documented in the beneficiary’s medical records:
- Beneficiary date of birth;
- Actual pack - year smoking history (number);
- Current smoking status, and for former smokers, the number of years since quitting smoking;
- Statement that the beneficiary is asymptomatic (no signs or symptoms of lung cancer); and
- National Provider Identifier (NPI) of the ordering practitioner.
- For the initial LDCT lung cancer screening service: a beneficiary must receive a written order for LDCT lung cancer screening during a lung cancer screening counseling and shared decision making visit, furnished by a physician (as defined in Section 1861(r)(1) of the Social Security Act) or qualified non-physician practitioner (meaning a physician assistant, nurse practitioner, or clinical nurse specialist as defined in §1861(aa)(5) of the Social Security Act). A lung cancer screening counseling and shared decision making visit includes the following elements (and is appropriately documented in the beneficiary’s medical records):
Reading radiologist eligibility criteria:
- Board certification or board eligibility with the American Board of Radiology or equivalent organization;
- Documented training in diagnostic radiology and radiation safety;
- Involvement in the supervision and interpretation of at least 300 chest computed tomography acquisitions in the past 3 years;
- Documented participation in continuing medical education in accordance with current American College of Radiology standards; and
- Furnish lung cancer screening with LDCT in a radiology imaging facility that meets the radiology imaging facility eligibility criteria below.
Radiology imaging facility eligibility criteria:
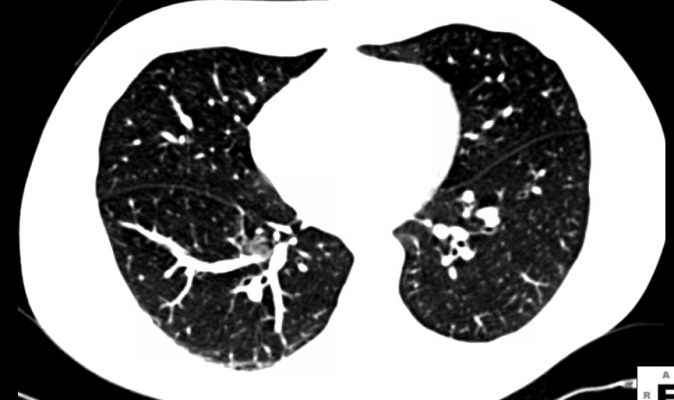
- Performs LDCT with volumetric CT dose index (CTDIvol) of ? 3.0 mGy (milligray) for standard size patients (defined to be 5’ 7” and approximately 155 pounds) with appropriate reductions in CTDIvol for smaller patients and appropriate increases in CTDIvol for larger patients;
- Utilizes a standardized lung nodule identification, classification and reporting system;
- Makes available smoking cessation interventions for current smokers; and
- Collects and submits data to a CMS-approved registry for each LDCT lung cancer screening performed. The data collected and submitted to a CMS-approved registry must include, at minimum, all of the following elements:
| Data Type | Minimum Required Data Elements |
|---|---|
|
Facility |
Identifier |
|
Radiologist (reading) |
National Provider Identifier (NPI) |
|
Patient |
Identifier |
|
Ordering Practitioner |
National Provider Identifier (NPI) |
|
CT scanner |
Manufacturer, Model. |
|
Indication |
Lung cancer LDCT screening – absence of signs or symptoms of lung cancer |
|
System |
Lung nodule identification, classification and reporting system |
|
Smoking history |
Current status (current, former, never). |
|
Effective radiation dose |
CT Dose Index (CTDIvol). |
|
Screening |
Screen date
Initial screen or subsequent screen
|
All CMS-approved registries must have the capacity and capability to collect data from any Medicare-eligible imaging facility/department that furnishes lung cancer screening with LDCT, with a catchment area that includes all 50 States, United States Territories, and the District of Columbia. CMS will evaluate each entity interested in participating as a CMS-approved registry to determine if they are capable of meeting the registry and data collection requirements outlined in this national coverage determination, including:
- Establishment of a steering committee and a governance board for oversight of the registry;
- Registry management plan, including identification of key personnel;
- Operational plan and framework that describes mechanisms for collection and submission of data from imaging facilities to the registry;
- Registry catchment area;
- Mechanisms for the submission of registry data to CMS electronically;
- Mechanisms to collect information (e.g.; HICN) in order to permit linkage of registry data with external databases (e.g. Medicare claims data sets);
- Description of data management and data quality review methods, including validation;
- Use of CMS-approved standardized data dictionary;
- Mechanisms for submitting a list of facilities participating in the registry to CMS; and
- Quality assurance plan.
To apply to function as a CMS-approved registry, interested entities must submit a letter of interest along with detailed supporting information about how the interested entity is able to meet the requirements outlined in this national coverage determination to the following address or via email to [email protected].
For more information:http://www.cms.gov/medicare-coverage-database/details/nca-decision-memo…


 February 09, 2026
February 09, 2026 









