A new statement to help physicians inform women on how breast density affects breast cancer screening and cancer risk has been issued by the American Society of Breast Disease.
"We applaud the strong support for more effective breast screening that new breast density state legislation provides women and their physicians, said Stephen A. Feig, M.D., FACR, ASBD's president. "ASBD's new guidelines will help women and their doctors better understand the issues around breast density and how they can make better informed decisions about breast cancer screening."
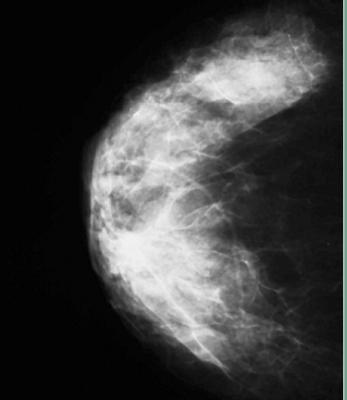
Breast density is determined by a mammogram. It is a measurement that compares the area of breast and connective tissue seen on a mammogram to the area of fat.
Breast cancer screening can involve additional tests beyond basic mammograms, especially for women who have an increased lifetime risk for breast cancer or dense breasts or both. For example, a physician might advise a woman with an elevated lifetime breast cancer risk and dense breasts to receive a whole-breast ultrasound in addition to a screening mammogram. A woman with a greater lifetime risk might be advised to receive a breast MRI in addition to a screening mammogram.
ASBD believes that if women know their lifetime risk (which is expressed as a percentage) and whether or not their breasts are dense, they will be better equipped to understand the recommendations their physicians make -- and make more informed screening decisions.
"Adults today are expected to know their blood pressure numbers and their blood cholesterol levels so they can make sensible lifestyle and medical decisions," said Sandhya Pruthi, M.D., ASBD's secretary-treasurer and past director of the Mayo Clinic's Breast Diagnostic Clinic. "It's just as important for adult women to know their lifetime risk for breast cancer and their breast density. And just like blood pressure or cholesterol levels, these numbers change over time." A helpful risk calculation model to assess lifetime risk is the Tyrer-Cuzik model and can be used to determine need for breast MRI screening.
Once a woman reaches the age of 40, her lifetime risk for breast cancer tends to drop each year that passes without the disease occurring. A woman's breast density will also tend to decline over time with decreasing estrogen production in the body with the transition to menopause.
Circumstances can reverse these tendencies, however. For instance, if a close family member is diagnosed with breast cancer, a woman's lifetime risk might raise, not drop, even though the woman herself had gone another year without the disease.
Breast density, a standard element in a patient's mammogram report, is an important factor in breast cancer screening because:
1) Dense breasts make a screening mammogram potentially less sensitive because the cancer may be obscured by the background breast density.
2) By itself, breast density increases lifetime breast cancer risk by about 3-4 times compared to women who does not have a dense breast pattern on the mammogram.
For these reasons, breast density has emerged as an important criterion in breast cancer screening, and has been the subject of legislation in several states.
Five states now mandate that breast density results be communicated to patients in a "patient's results letter." These states (California, New York, Virginia, Connecticut, and Texas) encompass 30% of the nation's women. Similar legislation is being considered in more than a dozen other states, and Congress is considering a federal law on the subject.
"In our view, breast cancer screening today is best seen as a multidisciplinary process, not a single test," said Stephen A. Feig, M.D., FACR, ASBD's president. "As part of this process, we support women being informed participants, with their primary physicians and their OB-gyn specialists, in their breast health decisions. Besides making women more satisfied patients, this leads to better compliance and better outcomes."
Breast cancer risk is determined by weighing several factors together. Among those factors are such criteria as chronological age, age at the time of first menstrual period, age at the time of first live birth of a child, previous diagnosis of breast disease, family history of breast cancer, ethnicity, and breast density.
"We have more effective methods than ever for detecting breast cancer," said Richard Reitherman, Ph.D., M.D., an ASBD board member and author of a tool for making breast cancer screening decisions based on breast density and lifetime risk. "For those methods to be used in the most effective way possible, women and their physicians have to work closely together in making breast screening decisions. This can only happen if women have better information about their cancer risk and the density of their breasts."
About the American Society of Breast Disease
Formed in 1976, the ASBD is a professional medical society that advocates the multi-disciplinary team approach to breast healthcare and educates physicians who strive to optimize breast health. The ASBD also supports a national breast disease research agenda, and otherwise collaborates with other scientific societies and advocacy organizations on breast health-related issues.
For more information: www.asbd.org


 February 18, 2026
February 18, 2026 









