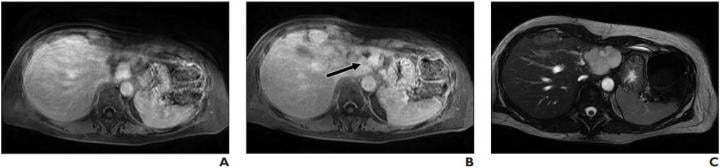
Lesion was originally reported as indeterminate enhancing mass, and outside report recommended biopsy. Classic features of benign hemangioma are shown. Error was attributed to faulty reasoning. A, Axial MR image obtained 5 minutes after contrast agent administration shows peripheral nodular discontinuous enhancement. B, Axial MR image obtained 10 minutes after contrast agent administration shows centripetal progression of enhancement (arrow). C, Axial fast imaging employing steady-state acquisition (FIESTA) MR image shows lesion is homogeneously hyperintense compared with liver parenchyma. Image courtesy of American Roentgen Ray Society (ARRS), American Journal of Roentgenology (AJR)
October 21, 2020 — According to an article in ARRS' American Journal of Roentgenology (AJR), secondary interpretations of body magnetic resonance imaging (MRI) at tertiary care centers identify a high rate of discrepancies — with primary errors being interpretive in origin — suggesting that subspecialty interpretations should be encouraged, and institutions should provide adequate resources for these interpretations to occur.
"We retrospectively identified 395 secondary MRI reports from January 2015 to December 2018 that were labeled as body MRI examinations at a tertiary care center," explained lead author Danielle E. Kostrubiak from the University of Vermont Medical Center.
After exclusions for erroneous categorization and no extant outside report, Kostrubiak and colleagues compared the outside reports with the secondary interpretations, categorizing cases as either discrepancy or no discrepancy. Subdividing the discrepancies according to the most likely reason for error via previously published categories, these categories were further divided into perceptive and cognitive errors.
"Of the 357 cases remaining after 38 exclusions," Kostrubiak et al. wrote, "246 (68.9%; 95% CI, 63.8-73.7%) had at least one discrepancy between the original outside report and the secondary interpretation provided at our institution."
The most common error type contributing to both overall and primary discrepancy was faulty reasoning (a cognitive error characterized by misidentifying an abnormality), which occurred in 34.3% of the total discrepancies (95% CI, 29.0- 40.0%) and 37.8% of the primary discrepancies.
The most common error type contributing to a second discrepancy was a type of perception error called satisfaction of search, which occurred in 37.0% of the second discrepancies and 15.0% (95% CI 11.2- 19.6%) of the overall discrepancies.
"We are not aware of any studies that have specifically focused on secondary interpretations of body MRI analyzed by type of likely error, and to our knowledge, ours is the largest MRI sample size published to date," the authors of this AJR article concluded.
Although the innate subjectivity of error classification stands to limit similar studies, Kostrubiak and team acknowledged that related research should become progressively easier to conduct as medical practices adopt more detailed electronic medical records.
"The next step," they wrote, "would be to explore how these discrepancies may impact patient outcomes and overall cost to the system associated with these radiologic errors."
For more information: www.arrs.org


 February 16, 2026
February 16, 2026