
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
Will PET/MR Ever Be Widely Adopted?
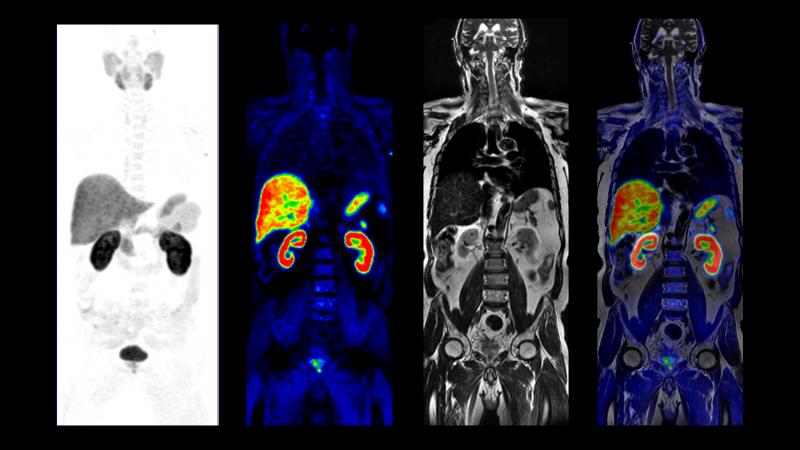
PET/MR images courtesy of GE Healthcare
In the world of molecular imaging, PET/MR is a wild card. But it’s a wild card that’s ready to be played. Three major vendors offer commercial products. The images are spectacular. So…what’s the hold up?
Probably more than anything, it’s the presence of positron emission tomography/computed tomography (PET/CT). And the fact that PET/CT has dug in.
It has to be frustrating for technophiles who have watched as engineers have overcome monumental challenges, notably hurdles to the simultaneous acquisition of PET and magnetic resonance (MR) data. Doing so demanded the development of solid-state PET detectors to replace the photomultiplier tubes that MR used to scramble with its magnetic field.
But despite this feat of engineering, it’s pretty much tit-for-tat clinically. PET/MR has been shown to be comparable to PET/CT in the detection of cancer. But there is a dearth of peer-reviewed research supporting its superiority over PET/CT. Further dragging PET/MR down are technical limitations affecting attenuation correction and the ability of PET/MR to operate within existing workflows. (More on these two later.) But first, let’s note that PET/MR has very good points in its favor.
One of the most important is its lack of ionizing radiation, a big plus when it comes to pediatric imaging, particularly of children who must be monitored for the recurrence of cancer for the rest of their lives. The accumulated X-ray burden for these patients is tough to bear.
Apples to apples (anatomically speaking). Also working in the favor of this hybrid are the exquisite images possible at 3T, the field strength of all commercial PET/MRs. On the basis of just MR versus CT, the answer would seem to lean toward PET/MR thanks to the superior soft-tissue contrast delivered by MR. Might one expect, then, that PET/MR would be preferable when visualizing the brain? Might this extend to the head and neck, abdominal and pelvic tissues, heart and musculoskeletal system?
But counterbalancing this advantage is PET/MR’s Achilles’ heel — attenuation correction (AC). Whereas PET/CT uses X-ray-based correction, PET/MR must rely on MR. With its limited field of view and dependence on bone for AC calculations, MR is a poor substitute for CT when it comes to calculating attenuation coefficients.
Time-of-flight PET might be leveraged to mitigate the problem. And other engineering sleights of hand could be in the offing, ones we can’t yet see. Therefore, it may be too soon to rule out PET/MR, on the basis at least of this one issue.
Workflow problems. Unfortunately for PET/MR lovers, even if future developments can overcome technical challenges associated with AC — and clinical research someday shows PET/MR definitively superior to PET/CT — there are workflow issues. Acquisition times for PET/MR vary depending on MR pulse sequences. In some instances PET/MR scans, therefore, will be longer than would ones completed with PET/CT, raising issues of how PET/MR can fit into the established workflow. But, again, there may be ways around this problem.
At issue is how to acquire MR data within the time allotted for bed positions assigned for the acquisition of PET data. These bed positions typically range from two to five minutes. Recent progress in developing ways to accelerate MR acquisitions suggest that MR data might be captured within those time windows.
The bottom line for PET/MR then may be written by the market forces that rule molecular imaging. And that could be problematic. PET/CT has struggled for more than a decade. A surge in demand for PET scanners in the early 2000s gave way after a few years to saturation and, ultimately, what is today a replacement market. Unless a strong case can be made for the use of PET/MR over PET/CT, there appears little chance that this alternative hybrid will gain traction.
But there are intangibles, most obviously those related to patient interests. The lack of ionizing radiation is an obvious one. And in the context of value medicine, this must be reconsidered, particularly as it relates to pediatric imaging. This is, however, a less compelling driver, given the dramatic reductions in dose that have been achieved lately in CT.
So the debate comes full circle, dropping the fate of PET/MR into the lap of clinical utility. This relates naturally to the context of MR’s advantages over CT and the advantage of PET/CT over PET/MR in regard to attenuation correction.
With no clear winner, it is likely that inertia will prevail. PET/CT will remain the go-to modality for molecular imaging, at least in the foreseeable future.
And PET/MR, despite impressive clinical results and engineering advances, will remain the wild card.
Editor’s note: This is the fourth blog in a series of four by industry consultant Greg Freiherr on Where Molecular Imaging Fits in Managing the Cancer Patient. To read the first blog, “How to Achieve the Quantitative Promise of PET/CT,” click here. To read the second blog, “Why the Use of PET/CT in Radiation Therapy Requires Thinking Outside the Box,” click here. To read the third blog, “Why Politics (and Money) Will Define the Next Generation of Scanners,” click here.


 January 28, 2026
January 28, 2026 









