Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
Why - And How - Digital PET Is Better Than Analog
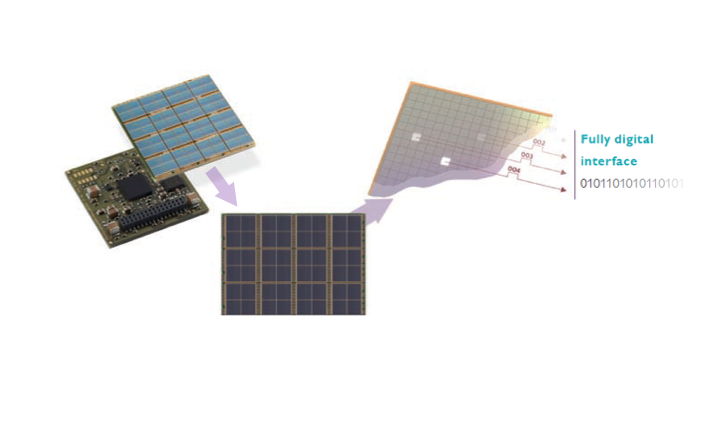
Each digital photon counter in the Vereos PET/CT detector contains thousands of solid-state sensors that digitally count individual photons.
Analog is approximate. Digital is specific. Therein lies the fundamental difference between digital PET and its analog cousin.
We see this difference every day in clocks, one displaying numbers, the other telling time with big and little hands. Digital and analog versions of PET are like that, but much more sophisticated, according to Michael A. Miller, Ph.D., a physicist at Philips Healthcare.
The digital photon counting detector, which is the backbone of Philips’ Vereos PET/CT, uses solid-state sensors to count the individual scintillation photons created during a PET scan. Analog PET detectors cannot count individual photons. Instead these detectors, which are built into the vast majority of installed PET/CTs, record flashes of light.
If lettuce farmers used similar technologies, their digital detectors would count the leaves of lettuce. Analog detectors would count the heads. When applied to clinical medicine, exactness translates into options, said Miller, who specializes in CT and advanced molecular imaging.
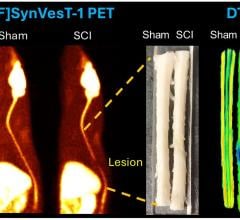
Vereos can be used to increase the quality of patient images compared to those obtained with analog PET/CT, making lesions easier to detect (see the blog, “How Digital PET/CT Can Improve Clinical Care”). Alternatively, the digital PET/CT might maintain image quality achieved over a substantially reduced scan time, as low as one-third or less of the typical 10 to 15 minutes. Or, physicians — exercising their knowledge and expertise to practice medicine — might choose a third option: to maintain image quality and scan time but reduce the dose of radiopharmaceutical injected into the patient.
“The detector allows us to get better data and do better corrections,” Miller said. This, in turn, creates higher quality images.
How PET Works
Regardless of whether the detector is digital or analog, PET imaging operates on the same principles. Positrons released by a radiopharmaceutical injected into a patient create high-energy photons. When these photons crash into scintillation crystals in the detector, they are converted into optical ones. This is where the type of detector matters.
The digital detector in Vereos counts optical photons individually. “With one-to-one coupling between the scintillation crystals and the digital sensors, there are many channels, each with a relatively low count rate. So we end up with good count rate performance,” Miller explained.
The resulting accuracy supports enhanced performance in time of flight (TOF) calculations, Miller said. These, as the name implies, reflect the millionths of a second in which the high-energy photons are in flight and provide the basis for determining the locations of the radiopharmaceutical in the patient’s body.
Consequently, Vereos excels at helping physicians detect cancer, which typically involves the radiotracer, fluorodeoxyglucose (F-18 FDG). Labeled with fluorine-18 radioisotope, this glucose molecule is the “go-to” radiopharmaceutical when using PET/CT for its most common applications, the detection of cancer. This is because cancer cells, which are hypermetabolic, consume glucose more rapidly than healthy tissue. This causes the accumulation of extraordinarily large amounts of the fluorine radioisotope in cancerous lesions.
PET images represent the distribution of FDG in the patient’s body. The context for these images — like the map underlying the GPS location of a car — is provided by a high-resolution CT scan of the patient, which also provides data about the attenuation of photons, information used to produce PET images.
PET/CT History
The first hybrid PET/CT scanner was introduced and evaluated clinically in 2000. But PET itself goes back to the early 1970s, when photomultiplier tubes were used to record scintillation flashes. Today many installed PET/CTs rely on this inherently analog technology.
By contrast, Vereos uses digital technology. Data for its PET images are obtained from solid-state silicon tiles, which are arranged in a many-sided polygon that encircles the patient. Light sensors and data processing arrays are hardwired into these tiles. Putting them together makes photon counting fast, accurate and free from the electronic noise produced in analog systems.
This lack of noise stems from the binary signal created by Vereos’ detector. The signals require no amplification, because the data are processed on the tiles themselves. And, because the signals are digital, they need not be converted from analog. Together, these attributes produce a high signal-to-noise ratio.
While the exactness possible with Vereos is dependent on the detector, “there are a lot of other pieces that come in,” Miller said. These multiple elements, working together, produce “really excellent image quality.”
For example, he said, the digital architecture of the scanner allows automatic and regular calibration. It also affords stability and consistency, which assures users that differences between current and prior images are not due to variability in the PET/CT.
“Vereos’ consistency is to the level where people don’t have to be concerned about it,” Miller said. “That improves clinical confidence.”
Digital imaging provides another benefit. Because PET images are digital, they can be easily fused with ones from CT. This fusion offers substantial advantages to physicians interpreting these images. (See the blog, “How Digital PET/CT Can Improve Clinical Care.”)
Together with the digital capabilities that come from digital photon counting technology, as well as the processing and calibration, Vereos delivers images that are uniform throughout, he said. For this reason, activity concentration and standardized uptake values (SUVs) can be measured accurately.
“Vereos achieves high imaging performance, which supports clinical needs and is facilitated by (digital) technologies,” said Miller, who puts Vereos at the apex of the PET/CT hierarchy. “It really gives people what they’re looking for when they want it — without any questions.”
Editor's note: This is the second blog in a series of four on digital PET/CT. The first blog, “How Digital PET/CT Can Improve Clinical Care,” can be found here.


 January 27, 2026
January 27, 2026