
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
How Digital PET/CT Can Improve Clinical Care
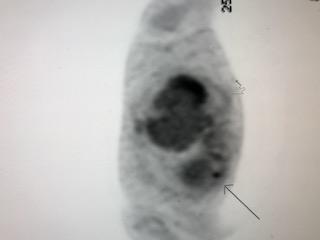
Digital PET/CT, achieved using Vereos from Philips Healthcare, can spot even a small lesion (arrow). Image courtesy of Brian Gordon, M.D.
PET/CT can be indispensible as a diagnostic and prognostic tool; in the assessment of patient response to therapy and cancer recurrence; even in the choice of therapy. And the significance of this hybrid imaging modality could grow in future years.
Digitalization is increasing the medical value of PET/CT, according to Brian Gordon, M.D., who interprets the majority of digital PET/CTs performed at the WellStar Kennestone Cancer Center in Marietta, Ga.
“An improved patient experience is the major advantage of digital PET/CT,” said Gordon, head of Nuclear Medicine for Quantum Radiology, a subspecialty radiology group that interprets images for the sprawling WellStar Health System.
The digital detector built into the Vereos PET/CT from Philips Healthcare improves sensitivity and, consequently, the detectability of small lesions. And it does so while reducing scan time.
“We have seen a significant decrease in scan time,” he said. “About a third of the scan time has been removed.”
Patient First
The result is an enhanced patient experience, according to Gordon. The Vereos replaced an analog PET/CT at the WellStar Kennestone Cancer Center in November 2017. Since then, PET/CT scan volume has reached as high as 18 patients per day.
Despite the high throughput, which ranges from this peak to about a dozen scans per day, scan accuracy is excellent, he said.
The WellStar Kennestone Cancer Center is one of the busiest PET/CT providers in the state of Georgia, he said. The digital detector has dropped scan times for whole body exams from 50 to 30 minutes and ones from the base of the skull to mid-thigh from 30 to 20 minutes.
The vast majority of scans at the center are oncologic. Many are ordered to evaluate suspicious lesions that were spotted initially on CTs or MRIs, but Vereos is also used extensively to monitor patient response to cancer therapy and to look for cancer recurrence.
Although shorter scan times have boosted throughput at the cancer center and improved the patient experience, accuracy is the top priority, Gordon said. The increased sensitivity of the digital detector improves image quality, while short scan times make the patient more comfortable and less prone to move. This reduces the likelihood of motion artifacts that can degrade images.
The short scans do not reduce image quality, Gordon emphasized. On the contrary, compared with analog PET/CT that operated before Vereos, he said, “we are able to detect activity in smaller lesions.”
The ability to detect very small lesions is critically important when PET/CT is applied in staging or monitoring. This is where the digital detector excels, according to Philips’ Director of Clinical Science for Nuclear Medicine Piotr Maniawski.
“Digital technology allows us to improve small lesion detectability,” said Maniawski who has worked in nuclear medicine for more than three decades, mostly at Philips Healthcare.
Digital PET/CT is well suited to find recurrent disease and characterize patient response to therapy, while providing the option of fast scans, he said.
Transition to Digital
The difference digitalization can make is apparent during tumor boards at the WellStar Kennestone Cancer Center. Vereos delivers digital PET images, which can be fused with ones from CT, Gordon said. These colorized, fused images “improve the discussion because the clinicians can see what I am talking about,” he said.
Clear communication is especially important when planning patient management in tough cases, when therapy choices are not straightforward, he said, as exemplified when deciding whether a lesion may be resectable or if radiation or chemotherapy should be administered first. “If you can localize exactly where (the lesion) is, you can make better decisions,” Gordon said.
The clinical benefits possible with the digital photon counting detector built into the Vereos PET/CT could become even more significant in the future, Maniawski said.
The clinical prospects of PET/CT are derived from the relative certainty possible with the digital detector, Maniawski said. But academic science advances cautiously.
Several collaborative projects between Philips and academic centers are underway using Vereos “to deliver clinical proof not only for competitive differentiation (digital versus analog) but also to push molecular imaging forward,” he said.
*Disclaimer: Results from case studies are not predictive of results in other case studies. Results in other case studies may vary.
Editor's note: This is the first blog in a series of four on digital PET/CT.
Related Content:
SPECIAL SUPPLEMENT: Examining the Value of Digital PET/CT



 February 16, 2026
February 16, 2026 









