May 25, 2021 — Independent verification always has been, and likely always will be, the core value proposition for RadCalc QA secondary check software. For more than two decades, this suite of widely deployed quality assurance (QA) tools has provided medical physicists and dosimetrists with fully automated and independent dosimetric verification of their radiotherapy treatment planning systems (TPS). What’s more, ongoing product innovation saw the RadCalc value proposition advance significantly last year with the clinical roll-out of automated 3-D dose-volume verification – a result of the successful integration of Monte Carlo and collapsed-cone convolution superposition algorithms into the platform.
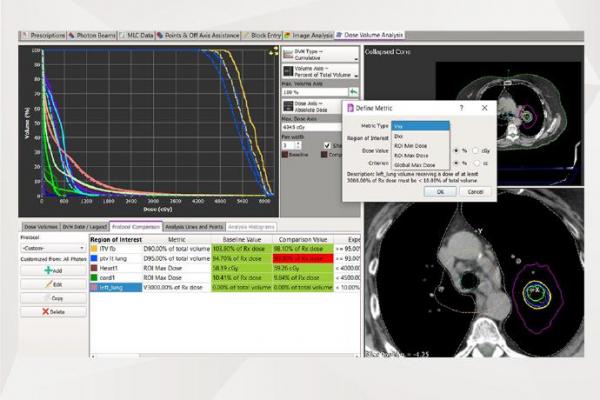
“With 3-D dose verification, we’re offering end-users a higher degree of certainty that the planning treatment volume is being validated, while assisting in the evaluation of plan quality by comparing dose to adjacent critical structures and organs at risk,” explained Craig Laughton, CTO and co-founder of the RadCalc software portfolio, part of LAP’s growing QA product line in radiotherapy. “That certainty translates into better targeting accuracy and dose distribution accuracy – and ultimately enhanced treatment outcomes – for the more than 2300 cancer centres that use RadCalc on a daily basis for patient QA.” As part of that QA workflow, all the physicist has to do is export a treatment plan via their DICOM RT and RadCalc will automatically verify the plan using either a Monte Carlo or collapsed-cone algorithm, generating results in minutes. If the treatment plan doesn’t pass various preset criteria, RadCalc will prompt the user to investigate what’s going on using a suite of dose analysis tools. “The user can slice-and-dice the plan just about any way they want by using our proven traditional workflows,” added Laughton, “while RadCalc’s new dependable features evaluate the cause of any discrepancies and determine the course of action.”
A 3-D take on patient QA
Among the early-adopters of RadCalc’s collapsed-cone convolution superposition algorithm are Joshua Robinson and colleagues at the James A Haley Veterans’ Hospital in Tampa, Fla. Robinson is one of four medical physicists within the clinic’s radiation oncology programme, overseeing a suite of three Varian treatment machines (including a new TrueBeam Edge system that’s currently being commissioned) and an Accuray CyberKnife treatment system, a robotic radiotherapy platform widely deployed in treating a range of disease indications using stereotactic radiosurgery (SRS) and stereotactic body radiotherapy (SBRT). “Our clinic supports cancer treatments across a predominantly male cohort of military veterans – so we see a lot of prostate, lung and head-and-neck patients,” explained Robinson. When it comes to patient QA, the James A Haley Hospital is a long-time RadCalc customer, with the product a key enabling technology in the “second-check everything” default setting of the radiation oncology department. “We like RadCalc functionality a lot – as well as all the support that comes with it,” Robinson added. “The software offers a powerful engine for second-check QA calculations, while the intuitive reporting integrates seamlessly into our clinical workflow.”
As a “lighthouse customer”, the Tampa clinic was among the first beta test sites chosen to evaluate RadCalc’s automated 3D dose-volume verification functionality – and specifically the software’s new collapsed-cone convolution superposition algorithm. The motivation, says Robinson, is to maintain confidence in the QA accuracy across harder-to-treat clinical indications – for example, small tumour targets surrounded by lung heterogeneities – as well providing independent QA checks across a range of advanced treatment modalities, including SRS, SBRT, intensity-modulated radiotherapy (IMRT), volumetric modulated-arc therapy (VMAT) and hypofractionation. “We’re still evaluating the collapsed-cone algorithm as part of our daily clinical practice,” noted Robinson. “One thing is already evident though: 3D dose verification increases your likelihood of getting a better, more accurate picture of dose distribution inside the patient. You’re doing the calculation on the planning CT – just like the TPS is doing the calculation on the planning CT – so you’re no longer just relying on a single dose point for the QA comparison.”
That’s especially important in more challenging treatment planning scenarios such as advanced head-and-neck cancers and late-stage prostate and rectal disease – indications that often require larger, heavily modulated treatment fields that are problematic in terms of conventional point-dose QA checks. Near term, Robinson sees the biggest clinical opportunity for 3D dose verification in the hospital’s lung SBRT patients, allowing treatment planners to accommodate the high dose per fraction while providing confidence in the steep dose gradients calculated by the TPS. ´“Depending on the size of the tumour and its location in the lung,” he noted, “a more complex planning technique is needed by the dosimetrists in order to achieve the steep dose gradients that minimize dose to the adjacent chest wall, heart and normal blood vessels. The Gamma Analysis and 3D comparison functionality in RadCalc help us to maintain confidence in the treatment plan along with our patient QA checks on the treatment machine.”
The QA roadmap
Right now, the RadCalc team is putting the finishing touches to the software roadmap for 2021 and beyond, including the imminent release of 3D EPID-based functionality to underpin true measurement-based IMRT QA and in vivo verification. In short, RadCalc will import the necessary EPID data/image files, process them, and then send to the collapsed-cone dose engine to calculate the dose. “The 3D EPID solution alongside delivery log file analysis will provide the most comprehensive patient QA solution on the market,” concluded Laughton. More broadly, RadCalc’s incorporation into the LAP group (in January 2019) has opened up new growth opportunities within the latter’s evolving product portfolio for radiation therapy. LAP’s offering for radiotherapy customers currently comprises laser systems for patient positioning, a suite of QA software and phantoms, as well as specialist beam-shaping technologies.
For more information: https://physicsworld.com/


 February 04, 2026
February 04, 2026 









