September 28, 2017 — Radiation therapy following mastectomy for intermediate-stage, high-risk breast cancer can be shortened from five to three weeks while maintaining tumor control rates in the breast and surrounding region that are equivalent to conventional treatment, according to new research. The findings were presented at the 59th Annual Meeting of the American Society for Radiation Oncology (ASTRO), Sept. 24-27 in San Diego.
Five-year results of a Chinese clinical trial with more than 800 post-mastectomy breast cancer patients confirmed that tumor recurrence rates following 15 daily fractions of radiation delivered over three weeks were not inferior to those following 25 fractions. Patients also experienced fewer side effects following accelerated treatment, indicating that hypofractionated radiation following mastectomy is a safe and effective treatment for locally advanced disease.
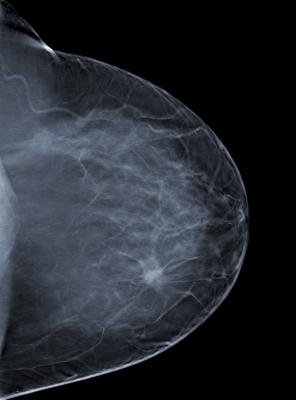
“Patients with invasive breast cancer receive radiation therapy after tumor-removal surgery to destroy any remaining cancer cells and prevent this very aggressive disease from returning,” said Shulian Wang, M.D., one of the study’s lead authors and a radiation oncologist at the Chinese Academy of Medical Sciences in Beijing, China.
“This trial demonstrates that we can safely accelerate adjuvant radiation therapy and reduce treatment time by two weeks. This option makes treatment more convenient for patients, reduces medical expenses and allows providers to treat more patients with limited resources.”
Of the 820 patients with high-risk breast cancer who enrolled in the trial from 2008 to 2016, 810 were eligible for analysis. The median age was 49 years (range 24-74 years). Nearly all patients (93.9 percent) had stage III breast cancer, and the remaining 6.1 percent had stage II disease.
All patients underwent mastectomy and received chemotherapy consisting of taxanes and/or anthracycline-based regimens (specifically, 88.6 percent taxanes and anthracycline, 8.9 percent taxanes-based, 1.9 percent anthracycline-based and 0.6 percent unknown), and some patients received trasuzumab targeted therapy (16.8 percent) and/or hormonal therapy (76.5 percent of all patients; 94.5 percent of those eligible). Patient and disease characteristics did not differ significantly between the treatment groups.
Following mastectomy, patients were randomly assigned in even proportions to receive either accelerated (i.e., hypofractionated) or standard (i.e., conventionally fractionated) external beam radiation therapy to the chest wall and supra-infraclavicular nodal region. The accelerated regimen consisted of 43.5 Gray (Gy) delivered in 15 fractions over three weeks, and the standard regimen consisted of 50 Gy delivered in 25 fractions over five weeks. Treatment was delivered via two-dimensional radiation therapy. Median follow- up for surviving patients was 55 months, with an interquartile range of 36 to 79 months.
At five years following accelerated treatment, the rate of locoregional recurrence, where disease returns in the breast or region near the breast, was noninferior to the rate for standard treatment. Locoregional recurrence rates were 8.3 percent following accelerated treatment and 8.1 percent following standard treatment (Hazard Ratio (HR) = 1.10, 95 percent CI 0.67-1.83), with a difference of 0.2 percent (95 percent CI = -4.1 to 4.5).
Among all patients, the five-year overall survival rate was 84.4 percent, and the disease-free survival rate was 72.7 percent. Five-year overall survival rates were 83.2 percent following accelerated treatment and 85.6 percent following standard treatment (HR = 1.13, 95 percent CI 0.78-1.62). Five-year disease-free survival rates were 74.6 percent for the accelerated treatment arm and 70.7 percent following standard treatment (HR = 0.88, 95 percent CI 0.67-1.16).
Rates of distant metastases, where a patient develops tumors outside the region of the original tumor, were 23.2 percent and 26.2 percent at five years for accelerated and standard treatment, respectively (HR = 0.90, 95 percent CI 0.67-1.20). Survival and recurrence rates were calculated using the Kaplan-Meier method and analyzed using Cox regression models.
The two cohorts did show some differences in terms of treatment-related side effects. Fewer patients in the accelerated treatment group experienced grade 3 acute skin toxicity (3.5 percent versus 7.8 percent of standard- treatment patients; p = 0.008). Rates between the treatment arms were similar for symptomatic radiation pneumonitis, lymphedema and shoulder disorder, and no patients experienced brachial plexopathy. Toxicity rates were compared using Chi-square tests.
“Clinicians have seen clear benefits with accelerated radiation therapy to the whole breast after breast-conserving surgery but questions remain about its safety and effectiveness with treating nodal regions. Our trial demonstrates a similar benefit for intermediate-stage breast cancer after mastectomy, in that we reduced treatment time from five weeks to three weeks while preserving high rates of tumor control and tolerability,” said Wang.
“The accelerated approach also has practical value for patients. With fewer treatment sessions, patients spend less time away from work and family, enjoy lower transportation costs and, as our findings show, experience fewer side effects.”
For more information: www.astro.org
Related Content
Clinical Trials and Cutting-Edge Radiation Oncology Research to Be Featured at ASTRO 2017


 February 06, 2026
February 06, 2026 









