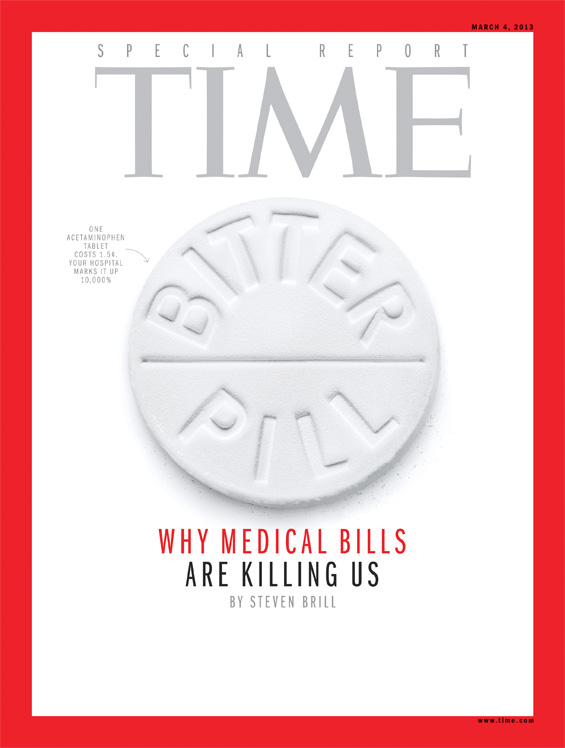
February 21, 2013 — Today, Time Magazine releases the dramatic findings of a months-long investigation by contributor Steven Brill into how outrageous pricing and egregious profits are destroying America's healthcare and creating even deeper budget deficits. The March 4, 2013 issue of Time goes on sale Friday, Feb. 22
Brill spent seven months analyzing bills from hospitals, doctors, drug companies and every other player in the American healthcare ecosystem, following the money to find out exactly how and why we are overspending, where the money is going and how to get it back. What he discovered will radically change the way you think about our medical institutions.
"With Obamacare we've changed the rules related to who pays for what, but we haven't done much to change the prices we pay,” Brill wrote. “When we debate healthcare policy in America, we seem to jump right to the issue of who should pay the bills, blowing past what should be the first question: Why exactly are the bills are so high? …Breaking these trillions down into real bills going to real patients cuts through the ideological debate over healthcare policy."
The 36-page investigation, the longest single piece ever published by a single writer in Time, reveals the shocking degree to which we enrich pharmaceutical companies, medical device makers, hospital administrators, laboratories and medical suppliers with lavish profits at the expense of patients. Brill explains that hospitals arbitrarily set prices based on inconsistent and subjective lists known as “chargemasters.” These prices vary from hospital to hospital and are often marked up as much as 10,000 percent the actual cost of an item. Seven patients' bills examined line by line for this article offer a close-up window into what happens when powerless buyers meet sellers in what is the ultimate sellers’ market. Katalin Goencz, a former appeals coordinator in a hospital billing department tells Time, “The hospitals all know the bills are fiction, or at least only a place to start the discussion, so you bargain with them."
Brill writes, "Unless you are protected by Medicare, the healthcare market is not a market at all. It’s a crapshoot. People fare differently according to circumstances they can neither control nor predict. They may have no insurance. They may have insurance, but their employer chooses their insurance plan and it may have a payout limit or not cover a drug or treatment they need. They may or may not be old enough to be on Medicare or, given the different standards of the 50 states, be poor enough to be on Medicaid. If they’re not protected by Medicare or they're protected only partly by private insurance with high co-pays, they have little visibility into pricing, let alone control of it. They have little choice of hospitals or the services they are billed for, even if they somehow know the prices before they get billed for the services. They have no idea what their bills mean, and those who maintain the chargemasters couldn’t explain them if they wanted to. How much of the bills they end up paying may depend on the generosity of the hospital or on whether they happen to get the help of a billing advocate. They have no choice of the drugs that they have to buy or the lab tests or computed tomography (CT) scans that they have to get, and they would not know what to do if they did have a choice. They are powerless buyers in a seller's market where the only sure thing is the profit of the sellers."
How to Fix it
Time Managing Editor Rick Stengel writes, "If the piece has a hero, it’s an unlikely one: Medicare, the government program that by law can pay hospitals only the approximate costs of care. It’s Medicare, not Obamacare, that is bending the curve in terms of costs and efficiency. Brill’s story is resolutely nonideological, but it resets the terms of one of our most important policy debates. Both sides of the aisle are culpable, as our elected leaders refuse to rein in hospitals and healthcare providers. According to Brill, there are things that can be done. He argues that lowering the age of Medicare entry, not raising it, would lower costs. And that allowing Medicare to competitively price and assess drugs would save billions of dollars. Asking wealthy Medicare recipients for higher co-pays would make sense. Most of all, healthcare must be a market in which patients can help control costs by understanding them better. And make sure you look at your hospital bill."
Drawing on a number of studies, Brill outlines a plan for $360 billion a year in potentials savings that would allow the United States to provide better care at lower costs:
1. Control prescription drug prices. The U.S. pays, on average, 50 percent more than other developed countries for the same drugs. Estimated savings: $94 billion
2. Recapture 75 percent of hospital profits and end the chargemaster. Ensure real competition and transparency at hospitals. Estimated savings: $84 billion
3. Limit the ordering of tests and other procedures sometimes used only to prevent medical malpractice lawsuits. Force lawmakers to enact medical-malpractice reform. Estimated savings: $74 billion
4. Regulate fees or tax profits on outpatient clinics. Estimated savings: $50 billion
5. Establish price controls on medical device makers. Bring overall gross profit margins down to 50 percent. Estimated savings: $30 billion
6. Allow and fund comparative-effectiveness evaluations in decisions to prescribe drugs, tests and medical devices. Estimated savings: $28 billion
Brill also reveals:
- The healthcare industrial complex spends more than three times on lobbying than what the military-industrial complex spends in Washington — $5.36 billion since 1998 compared to $1.3 billion spent by defense and aerospace interests in the same period.
- "We’re likely to spend $2.8 trillion this year on healthcare. That $2.8 trillion is likely to be $750 billion, or 27 percent, more than we would spend if we spent the same per capita as other developed countries, even after adjusting for the relatively high per capita income in the U.S. vs. those other countries."
- Tax-exempt “nonprofit” hospitals are the most profitable businesses and largest employers in their regions, often presided over by the most richly compensated executives.
- Cancer treatment — at some of the most renowned centers such as Sloan-Kettering and M.D. Anderson — has some of the industry’s highest profit margins. Cancer drugs in particular are hugely profitable. For example, Sloan-Kettering charges $4,615 for a transfusion of a plasma called Flebogamma. Medicare cuts Sloan-Kettering's charge to $2,123, still way above what the hospital paid for it, an estimated $1,400.
- Patients can hire medical billing advocates who help people read their bills and try to reduce them. Read more about how you can control your own costs: http://ti.me/UJSY1V
This week's TIME Special Report: Bitter Pill is in partnership with CNN. Tune in to Starting Point Thursday, Feb. 21 at 8:30 am and Anderson Cooper 360 at 8 and 10 pm ET to see Steven Brill explain his findings. Time Managing Editor Rick Stengel will also join Situation Room Thursday. Online, Time.com and CNN.com will be inviting users to share their own stories with medical costs. CNN iReport will ask readers to share their personal stories and TIME will feature some of the best on its site. Time.com will invite users to share their experiences in a live, blog-style commenting section and will compile social media interactions in real time using #BitterPill.
Watch video of Brill discussing his story: http://ti.me/WSuySj
Read the full story here: http://ti.me/15wrtfm


 February 06, 2026
February 06, 2026 









