Magnetic resonance imaging (MRI) is safe, profoundly safe, provided we follow industry best practices. Unfortunately, the rates of reported MRI accidents are nearly five times what they were just five years ago, according to data from the U.S. Food and Drug Administration (FDA)[1] — an apparent indication that we, as an industry, aren’t following best practices.
There are certain facility and operational standards that should be elemental to every MRI operation, and it is vital that imaging centers and departments ensure there is strict adherence to safety measures. The following list is a recap of standards and hazards to use as a guideline:
Zones
The American College of Radiology, in its 2007 “Guidance Document for Safe MR Practices,” describes a sequence of screening and access controls, called the Four-Zone model. It describes a process by which patients, personnel and equipment are required to pass clinical/physical screenings prior to being granted access to the areas immediately around the MRI scanner room. Some regulatory and accreditation bodies have become increasingly focused on the signage for these zones, but labeling an area “Zone III” is far less valuable than actually providing the protections that go with that designation.
The four zones are:
• Zone I – This is the outside world, i.e., areas that have nothing whatsoever to do with MRI.
• Zone II – This could be the reception or waiting area. This is the zone in which we screen persons and objects for their safety and suitability to approach the MRI scanner.
• Zone III – This is any area (beyond the MRI scanner room) where there is a potential magnetic field danger to persons, or any area from which there is access to the MRI scanner room. Zone III is to be physically restricted from Zone II, and persons in Zone III are to be under the continuous supervision of MRI personnel.
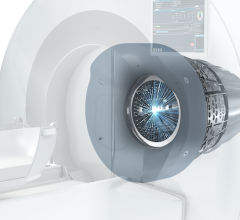
• Zone IV – This is the MRI scanner room itself, and this is where the risks are greatest. No person or object should ever be allowed into this room without both a comprehensive screening and direct supervision.
Burns
Perhaps the most frequent MRI adverse event is burns, which can arise from contact with the bore, large caliber body loops (thumbs-on-thighs are alarmingly common) or electrically conductive elements in the bore. Safety measures to avoid burns include:
• Pad the patient – If the patient is too large to fit in the bore with the indicated amount of padding between them and the RF elements, then the study should be reconsidered.
• Prevent skin-to-skin contact – Gowning patients is often recommended, but gowns can make it easier for skin-to-skin contact, such as medial thighs/ankles. Make sure the patient’s skin doesn’t touch, either through clothing, pads or blankets.
• Conductive elements – Anything extraneous to the study, such as ECG leads, should be completely removed from the patient. Any remaining leads, wires or cables should be run straight out the bore of the scanner and separated from the body of the patient by padding.
• Delayed action – Many MRI burns can’t be immediately detected or diagnosed, as they may take minutes, or even hours, to reveal themselves. Patients who complain of warming, itching or skin irritation, particularly in skin-to-skin contact areas, should be kept for observation.
Hearing Damage
While nearly every MRI facility provides earplugs, not every facility requires their use or instructs patients on the proper way to place them. Cramming brilliant yellow plugs in the far-outer ear will provide virtually no protection, and yet patients will appear to have appropriate hearing protection. MRI providers must instruct patients on how to use plugs and should offer alternative hearing protection for patients for whom the in-the-ear plugs don’t fit effectively.
Ferromagnetic Detection
The most infamous MRI accidents involve magnetic projectiles. Historically, it fell to the technologist to determine, for example, whether a portable oxygen cylinder is steel or aluminum or if a particular wheelchair (or ventilator or medication pump or mop bucket) was safe to be brought into the MRI scanner room.
New MRI facilities (or MRI facilities receiving new magnets) may now be subject to requirements of the 2010 edition of the “Guidelines for Design and Construction of Health Care Facilities” (the hospital building code), which require a facility to design elements from the above (as well as a number of others).
With the proper facility and operational protections, MRI can remain profoundly safe. We all should work to reverse the alarming trend of increasing accidents.
Tobias Gilk is senior vice president of RAD-Planning, a design consulting firm for medical imaging facilities, and president and MRI safety director of Mednovus, an MRI safety company. He has presented programs on MRI safety at American Healthcare Radiology Administrators (AHRA) and other venues.
Note: The FDA will hold a workshop on MRI safety, Oct. 25-26, in Silver Spring, Md., to discuss factors affecting the safe use of MRI and ways to mitigate risks, both for the patient and staff. A webcast and transcript of the workshop will be available online in mid-November. For more information: www.fda.gov/MedicalDevices/NewsEvents/WorkshopsConferences/ucm270720.htm
1. U.S. Food and Drug Administration, Manufacturer and User Facility Device Experience (MAUDE) database, www.accessdata.fda.gov/scripts/cdrh/cfdocs/cfmaude/search.cfm, using product code LNH and comparing reports for those years.

 March 09, 2026
March 09, 2026 









