A study examining trends in X-ray computed tomography (CT) use in children in the United States has found that reducing unnecessary scans and lowering the doses for the highest-dose scans could lower the overall lifetime risk of future imaging-related cancers by 62 percent. The research by a UC Davis Health System scientist was published in JAMA Pediatrics. It is accompanied by a journal editorial.
The 4 million CT scans of the most commonly imaged organs conducted in children each year could result in approximately 4,870 future cancers, the study found. Reducing the highest 25 percent of radiation doses could prevent 2,090 — or 43 percent — of these future cancers. By also eliminating unnecessary imaging, 3,020 — or 62 percent — of cancers could be prevented, said Diana Miglioretti, lead study author and Dean’s Professor in Biostatistics in the Department of Public Health Sciences at UC Davis Health System.
“There are potential harms from CT, meaning that there is a cancer risk, albeit very small in individual children, so it’s important to reduce this risk in two ways,” said Miglioretti, who is a member of the UC Davis Comprehensive Cancer Center. “The first is to only do a CT when it’s medically necessary, and use alternative imaging when possible. The second is to dose CT appropriately for children.”
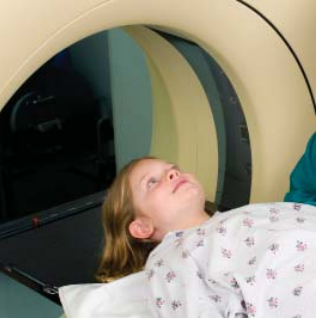
Computed tomography is a procedure used to generate cross-sectional images of the body in diagnostic and therapeutic settings. It frequently is used in young children who may have experienced trauma, for example. Miglioretti noted its use has increased dramatically because the technology is effective and offers greater convenience than other imaging methods that do not involve ionizing radiation, such as magnetic resonance imaging (MRI), which requires that a child remain still in a scanner for an extended period of time. Ultrasound imaging can be time consuming. Radiation doses delivered by CT are 100 to 500 times higher than for conventional radiography, Miglioretti said.
The retrospective study was conducted in diverse male and female children under 15 who were enrolled in seven integrated health-care systems: Group Health Cooperative in Washington; Kaiser Permanente in Colorado, Georgia, Hawaii, and the Northwest; and Marshfield Clinic in Wisconsin; as well as Henry Ford Health Systems in Michigan. Miglioretti conducted the research while employed at Group Health Cooperative, where she maintains a joint appointment.
The researchers examined CT utilization data from six of the health-care systems between 1996 and 2010. Radiation dosage and estimated cancer risk were calculated by examining 744 random CTs of the head, abdomen/pelvis, chest and spine conducted from 2001 through 2011 at five of the health systems. The researchers said exams from these regions of the body account for more than 95 percent of all CT scans.
Estimated lifetime attributable risks of cancers were calculated using the Biological Effects of Ionizing Radiation (BEIR) VII report for breast, colon, liver, lung, ovarian, prostate, stomach, thyroid, bladder, and uterine cancers and leukemia, and using models developed with similar methods for oral, esophageal, rectal, pancreatic, kidney and brain cancers, which account for as much as 85 percent of all U.S. cancer incidence.
The study found that CT use increased between 1996 and 2005. Among children under 5, CT use doubled from 11 in 1,000 in 1996 to 20 in 1,000 in 2005-2007, then decreased to 15.8 in 1,000 in 2010. Among children 5 to 14, CT use almost tripled, from 10.5 in 1,000 in 1996 to a peak of 27 in 1,000 in 2005 before decreasing to 23.9 in 1,000 in 2010. The researchers also found that patient radiation doses were highly variable for exams of the same anatomic region.
The risk of radiation-induced leukemia and brain cancers are highest for head CT, the most commonly performed CT in children. While the effective dose for head CT is relatively low, the brain and red bone marrow doses are relatively high for young children, resulting in the greatest risk of brain cancer and leukemia for imaged organs. The risk of radiation-induced solid cancer is highest for CTs of the abdomen and pelvis, which also had the most dramatic increase in use, especially among older children. Breast, thyroid and lung cancers and leukemia account for 68 percent of projected cancers in exposed girls; brain, lung and colon cancer and leukemia account for 51 percent of future cancers in boys.
Miglioretti explained that children’s organs are at an increased risk of cancer from CT scans because children still are growing and their cells are dividing rapidly. In addition, lifetime risk of cancer is greater among children because they are at the beginning of their lives — they have longer to live.
She noted that physicians can reduce dosage amounts using a number of different strategies, including reducing scan length by focusing solely on the ‘zone of interest’ — the region requiring imaging. For example, when the zone of interest is the abdomen, physicians should avoid also scanning the pelvis. She said dosage guidelines for imaging pediatric patients should be followed closely.
The Image Gently campaign, an initiative of the Alliance for Radiation Safety in Pediatric Imaging that encompasses the Society for Pediatric Radiology, American Association of Physicists in Medicine, American College of Radiology and American Association of Radiologic Technicians, aims to change practice by increasing awareness of opportunities to promote radiation protection in medical imaging of children.
“A smaller person needs a lower dose to come out of the machine to create an image of adequate quality for making a clinical diagnosis,” Miglioretti said.
The research was supported by grant # U19CA79689 from the National Cancer Institute Cancer Research Network Across Health Care Systems; grant #R21CA131698 from the National Cancer Institute; and grant #K24CA125036.
Other study authors include Rebecca Smith-Bindman, UC San Francisco; Eric Johnson of Group Health Research Institute; Andrew Williams, Center for Health Research, Kaiser Permanente, Hawaii; Robert T. Greenlee of the Epidemiology Research Center, Marshfield Clinic Research Foundation; Sheila Weinmann, Center for Health Research, Kaiser Permanente, Northwest; Leif I. Solberg, Health Partners Institute for Education and Research, Kaiser Permanente, Denver; Douglas Roblin, Center for Health Research, Kaiser Permanente, Southeast; Michael J. Flynn, Henry Ford Health System; and Nicholas Vanneman, Institute of General Practice, Johann Wolfgang Goethe University, Germany.
For more information: www.healthsystem.ucdavis.edu.


 March 06, 2026
March 06, 2026 









