January 22, 2013 — Using tiny balloons to temporarily block blood flow to the uterus during a high-risk Caesarean-section delivery can save the life of the mother while preventing hysterectomy and preserving fertility, suggests research being presented at the 25th annual International Symposium on Endovascular Therapy (ISET).
The placenta attaches abnormally in some pregnancies, putting the mother and baby at risk during delivery due to the likelihood of hemorrhage when the placenta is detached from the uterine wall. Women with this condition must undergo a C-section, but excessive blood loss remains a risk, and it may be necessary to perform a hysterectomy to save the life of the mother and baby. These women also have blood transfusions to replace the lost blood.
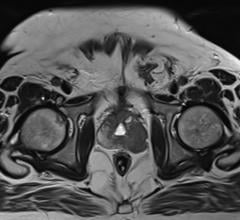
Called uterine artery balloon occlusion, the minimally invasive treatment involves inflating tiny balloons in the main arteries feeding the uterus (internal iliac arteries) prior to the C-section to stop the blood flow to the uterus. The research being presented at ISET suggests in particularly severe cases, it may be beneficial to perform an additional procedure, called uterine tamponade. Uterine tamponade involves inflating a special balloon to fill the inside of the uterus after the baby is delivered, using pressure to help control the bleeding.
“Before routine prenatal ultrasound, many of these women would die in childbirth, but now we can diagnose the problem in advance and plan to perform balloon occlusion before a scheduled C-section,” said Constantino Pena, M.D., medical director of vascular imaging, Baptist Cardiac and Vascular Institute, Miami, Fla., where many women have undergone the procedure. “In some difficult cases, we even use gel foam particles to temporarily embolize (block) the arteries to prevent bleeding. Internal iliac artery balloon occlusion is becoming more common, offering women a chance to preserve their fertility.”
In the study being presented at ISET, 35 pregnant women had uterine artery balloon occlusion prior to undergoing C-section; 24 of those women also had uterine tamponade. Twenty-six of the women had transfusions averaging 1,870 ml — far less than the usual blood loss of 3,000 to 6,000 ml for women with this condition. All of the women and infants survived. Seven of the women (18 percent) ultimately had hysterectomies. In some cases the placenta attaches so deeply into the wall of the uterus — a condition called placenta accreta — it becomes impossible to remove without life-threatening blood loss, and hysterectomy is the only option.
Balloon occlusion involves placing a thin tube, or catheter, via the groin artery (femoral artery), advancing it to both internal iliac arteries and inflating a tiny balloon in each prior to the C-section. The balloons remain in place during the C-section and for a period of time after the delivery if blood loss is severe. The balloon occlusion procedure is performed by an interventional radiologist. Uterine tamponade is performed by a gynecologist. Although it can help slow the bleeding, uterine tamponade often does not resolve the problem.
“Our research demonstrates that obstetricians and interventional radiologists should work together to maximize patient safety and save the life of the woman with an abnormal placenta. By partnering, they can reduce blood transfusions and related complications, including preserving the uterus,” said Azzam Khankan, M.D., Ph.D., an interventional radiologist at King Abdulaziz Medical City, Riyadh, Saudi Arabia, and lead author of the study. “This most likely will help ensure future fertility and the woman’s peace of mind.”
For more information: www.ISET.org


 July 25, 2024
July 25, 2024