
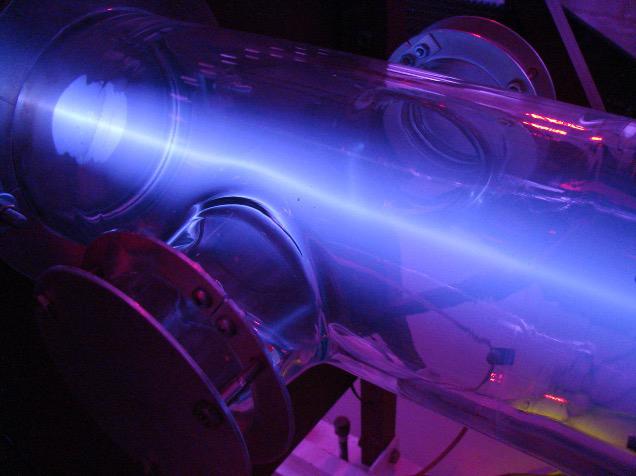
Shine Test System paired with the world’s strongest commercial fusion neutron generator manufactured by Phoenix. It can break apart low-enriched uranium to produce moly-99 for medical isotope production.
Medical imaging procedures such as single-photon emission computed tomography (SPECT) scans, myocardial perfusion scans and bone scans are used to diagnose issues such as heart disease and cancer, and deliver lifesaving treatment to tens of thousands of patients every day around the world. But the material that makes these procedures possible — a radioactive isotope of the element molybdenum referred to as “molybdenum-99” or simply “moly-99” — is in short supply.
These procedures depend on short-lived radioactive isotopes such as technetium-99m or fluorine-18 as tagging agents since they decay into stable and inert material so quickly that there is no risk of damaging the human body with radiation when ingested or injected into the bloodstream, and all of these isotopes are derived from moly-99. Today, only a handful of facilities produce the entire world’s supply, and a single facility ceasing production for just a few days leads to worldwide shortages. In order to mitigate and prevent future shortages, many companies, such as Phoenix LLC and Shine Medical Technologies, are developing new and more efficient ways to produce massive quantities of moly-99.
What Is Moly-99?
Molybdenum-99 is an isotope, which means it has more neutrons in its atomic nucleus than normal elemental molybdenum. Some isotopes are stable, but others are unstable, meaning that the atom cannot hold itself together and must expel particles and energy in order to transform into a more stable element. This process is called atomic decay. For example, moly-99 decays by releasing a beta particle (in other words, an electron) and transforming into technetium-99m, which itself decays far more rapidly into technetium-99, which itself decays far more slowly into stable ruthenium-99.
Every isotope has a different half-life or amount of time it takes for half of any given sample of any size to decay. Molybdenum-99 has a half-life of roughly 66 hours, so no matter how much of it you have at any given time, you will have half of that leftover after a little over two and a half days. Technetium-99m has a half-life of six hours, and therefore any amount that is introduced into your body for a medical scan has depleted by about 93 percent within 24 hours (this is what makes it so useful for medical imaging). Technetium-99, the byproduct of technetium-99m’s radioactive decay, though, has a half-life of 211,000 years, which it spends weakly emitting small amounts of beta radiation that poses little danger to the patient’s health before becoming stable ruthenium-99.
As a result of radioactive decay, there is no possible way to stockpile molybdenum-99 — or any other radioisotope with half-lives on the scale of days or hours. Facilities that produce moly-99 must constantly be producing it with the knowledge that all over the world, the supply of moly-99 constantly decreases. In fact, producers of technetium-99m and other medical radioisotopes must always buy as much as one-third more moly-99 than they need, depending on how far across the world the nearest moly-99 producer is, simply to account for the amount of moly-99 that will decay in transit.
Currently, the world’s supply of molybdenum-99 is produced in several specialized nuclear reactors. Moly-99 is a byproduct of the decay of fissile uranium, and so fission reactors, which split apart atoms of highly enriched uranium, produce large amounts of it. In the vast majority of nuclear reactors, moly-99 is more or less an irrelevant byproduct, since the primary function of the reactor is to produce kinetic energy that can be transformed into electricity. However, a few facilities around the world are specifically designed not to produce electricity, but rather to harvest moly-99. There are only five such facilities in the entire world, none of which are located in the western hemisphere.
New Ways to Produce Moly-99
Since even one of these four reactors shutting down even for a few days — for example, for temporary maintenance — imperils the world’s supply of molybdenum-99, world governments recognize the vital need for new ways to produce moly-99. Reactors have other downsides, too, such as their reliance on highly enriched uranium, which is difficult to transport for security reasons. Because of this, several companies have received financial aid from the government to develop ingenious new methods of moly-99 production for medical imaging that does not rely on highly enriched uranium.
Many of the new methods being investigated involve the use of particle accelerators, not fission reactors. For example, one method being looked into by NorthStar Medical Radioisotopes involves using particle accelerators to either add or subtract neutrons to or from naturally occurring and stable molybdenum-98 or molybdenum-100, respectively; another method being investigated by Niowave involves using an electron accelerator to split uranium atoms instead of a reactor.
One of the most promising companies in the race to revitalize moly-99 production is Shine Medical Technologies. Shine’s method for isotope production relies on the extremely powerful fusion neutron generators developed by its sister company Phoenix LLC to break apart uranium into molybdenum-99. These neutron generators are a near-term application of nuclear fusion, in which light elements such as deuterium, a stable hydrogen isotope, are fused to produce helium and neutron radiation. The neutron radiation, when interacting with uranium, causes the uranium atoms to break apart into lighter elements including moly-99. While nuclear fusion’s biggest claim to fame is its potential application as a source of clean energy, it has many other applications related to the production of neutron radiation, including not only isotope production, but also industrial radiography and materials analysis.
Phoenix’s neutron generators in Shine’s system allow for substantial amounts of the medical isotope to be produced out of comparatively smaller and less highly enriched amounts of uranium. This process uses low-enriched uranium (LEU) instead of highly enriched uranium (HEU), which is beneficial
for several reasons including safety and security. Shine’s production facility in Janesville, Wisc., is projected to be capable of supplying one-half of the entire United States’ demand for moly-99 when it comes online.
Opening Production Chains
Though hospitals in the United States make up half of the global demand for moly-99, there have been no facilities within the U.S. that produce moly-99 for over three decades now; the last facility in the entire western hemisphere to produce moly-99 shut down in January of 2019. The companies working to open up domestic moly-99 production are performing a key role in alleviating the burdens on the world’s supply chain for this lifesaving radioisotope. New facilities worldwide in the years to come aim to make crippling moly shortages, the most recent of which occurred in 2018 when three reactors were taken down for routine maintenance at once, a thing of the past.
Willow Ascenzo is a marketing copywriter and content creator for Phoenix LLC, a nuclear technology company headquartered in the Madison, Wisc., area.


 February 06, 2026
February 06, 2026 









