An example of Philips’ TrueVue technology, which offers photo-realistic rendering and the ability to change the location of the lighting source on 3-D ultrasound images. In this example of two Amplazer transcatheter septal occluder devices in the heart, the operator demonstrating the product was able to push the lighting source behind the devices into the other chamber of the heart. This illuminated a hole that was still present that the occluders did not seal. Photo by Dave Fornell
A new year — and decade — offers the opportunity to reflect on the advancements and challenges of years gone by and ponder the question: what’s next? For radiologists, constant innovations in medical technology mean the landscape may not look the same year over year, or certainly from decade to decade. At the 2019 meeting of the Radiological Society of North America (RSNA) in Chicago, three medical professionals with their finger on the pulse of radiology presented on different areas of innovation, from hybrid imaging procedures to artificial intelligence (AI). Read on for their insights.
Advanced Combination Imaging Procedures
During his talk at RSNA, Osmanuddin Ahmed, M.D., discussed the utilization of hybrid CT-fluoroscopy in interventional radiology. Ahmed is assistant professor of radiology in the division of vascular and interventional radiology at the University of Chicago.
Ahmed’s facility at University of Chicago recently acquired hybrid imaging technology from Canon that combines computed tomography (CT) and an angiography unit in one piece of equipment. While this Angio-CT technology has been around since the late-1990s in Japan, it still hasn’t quite taken off in the United States, and Ahmed said the unit at University of Chicago is one of just a handful being used in the U.S.
Angio-CT is essentially a CT scanner and angiography system that share a common patient bed, allowing radiologists to use fluoroscopy, CT or both. As for the benefits, Ahmed said the unit makes it easy to switch between CT and fluoroscopy in just minutes, improving efficiency and the patient experience.
“I think for a lot of interventionalists, when you have a procedure you think ‘OK, is this a CT procedure or is this an angiography or fluoroscopy procedure,’ and you make that decision very early on,” he said. “The beautiful thing about this technology is you don’t have to make that decision anymore,” Ahmed said.
With CT and fluoroscopy available in the same room, Ahmed said radiologists are equipped to handle all sorts of cases, from the everyday to those that are more advanced.
“I think that’s the most interesting thing about this technology, is that it’s not just for your one percent of cases,” he said. “It’s actually for the 99 percent of cases because you’re using it for your bread and butter stuff and you’re also using it for the occasional interesting or complex case that comes your way.”
Hybrid CT has especially significant impacts in the area of interventional oncology in particular, Ahmed said. As radio-embolization solidifies as a common modality of treating cancer, it becomes paramount that radiation is meticulously delivered to the tumor and not the surrounding areas. With hybrid CT imaging, Ahmed explained you can see very clearly exactly where you are treating from and identify sources of non-target embolization. Hybrid imaging also provides a highly accurate depiction of the volume of liver the radiation is being delivered so the appropriate dose can be administered.
Ahmed doesn’t see many drawbacks with hybrid CT technology, aside from cost, which he said has likely been a barrier to more widespread adoption. As for the future of this technology, Ahmed’s view is that it will start becoming more widespread. Twenty years from now, he expects it will be uncommon to see an IR suite that does not have a hybrid CT room.
“It’s a no-brainer. I think that the product speaks for itself,” he said. “It’s just a matter of getting it published and showing people what we can do with it.”
AI and Neuroimaging
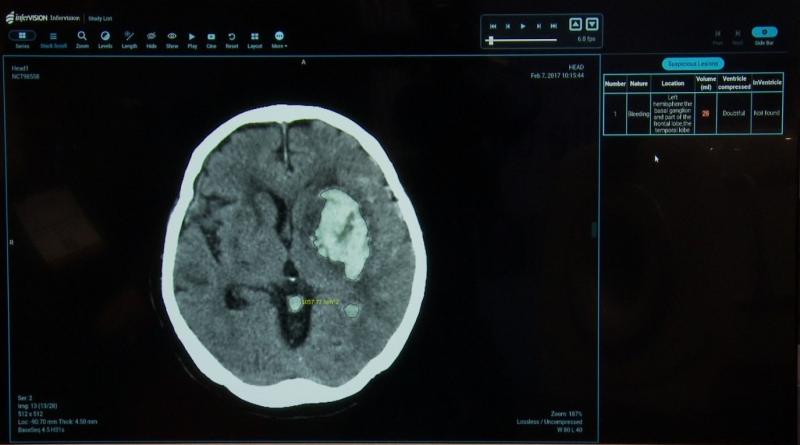
One look at the expanding AI Showcase at RSNA alone is telling enough of the future of AI as a tool for radiologists. At RSNA, Narayan Viswanadhan, M.D., spoke on the future of AI and its implications in the area of neuroimaging. Viswanadhan is the assistant chief of radiology at the James A. Haley veteran’s hospital in Tampa, Fla., and assistant professor of radiology at University of South Florida. In addition to his own clinical research on deep learning and radiology, he consults with AI company Zebra Medical on their products as they relate to brain bleeds and other areas.
Viswanadhan noted the explosion of AI technologies at RSNA 2019, estimating that AI comprised about 40 percent of the conference. In terms of applications for AI in the neuroimaging field, Viswanadhan is excited about the development of triage mechanisms that can detect brain hemorrhage and bring cases to the top of a radiologist’s worklist. He is also interested in AI technologies intended for stroke detection, with the development of emerging software tools that automatically detect large vessel occlusions and send alerts to the appropriate people on a stroke team.
With all of the hype surrounding AI, some have claimed in recent years that radiologists will eventually be replaced by the technology. Viswanadhan does not believe this is at all the case, especially given all that radiologists do.
“While the primary focus is on reading images, we also consult with physicians, we basically do procedures, and we also evaluate imaging in the framework of the clinical history and other relevant pieces of information,” he said.
Today, he sees the emerging AI technologies as falling within a more narrow scope, with the U.S. Food and Drug Administration (FDA) approving applications used for detection, but not diagnosis. The AI tools that have been approved so far each have their specific applications, like finding a hemorrhage or an occlusion. It is up to the radiologist to utilize these hyper-focused tools while also seeing the bigger picture.
As for the future of AI, Viswanadhan said many valid questions still remain around areas like ethics and cybersecurity, and there are still concerns with overfitting of data and the issue of biases in data sets and algorithms. As more regulatory frameworks are established, he expects more applications will slowly gain FDA approval, at which point it will be up to the medical community to evaluate the proper uses of the tools through evidence-based medicine. While this is no overnight process, it is clear that AI is here to stay — and so are radiologists.
While Viswanadhan does not see radiologists going anywhere soon, he does think it is fair to say that radiologists who don’t use AI tools will be replaced by radiologists who do. His recommendation to those in the field is not to fear AI and view it as a threat, but to see it as another supplement to their work.
“I think that radiologists, radiology trainees and medical students need to embrace this technology, and really familiarize themselves with understanding what exactly AI is, what is deep learning, how does this process work, what are neural networks — some of the basic definitions,” he said.
By familiarizing themselves with AI, Viswanadhan said, radiologists will be better equipped to evaluate emerging technologies and feel confident about the tools they choose to use.
Integrated 3-D Imaging
Joseph Vettukattil, M.D., MBBS, spoke at the conference on integrated 3-D imaging as the future of cardiac imaging. Vettukattil is co-director of the congenital heart center and division chief of pediatric cardiology at Spectrum Health Helen DeVos Children’s Hospital in Grand Rapids, Mich., where he leads the cardiac catheterization lab and clinical research team.
As an expert in 3-D echocardiography, he spoke on the uses of advanced imaging techniques for the management of patients with complex congenital heart defects. With the advancements of 3-D printing in recent years, cardiologists and surgeons have been able to make more informed interventional plans using 3-D models. Three-dimensional modeling has the potential to improve overall surgical outcomes while increasing the efficiency of procedures and ultimately decreasing radiation exposure.
When it comes to congenital heart disease, it is especially important for clinicians to have a detailed visualization of the pathomorphology of the heart for proper diagnosis and management in both children and adults. An accurate 3-D model can become an invaluable tool.
In a 2016 article in the Journal of Digital Imaging,¹ Vettukattil and others noted that while 3-D printing has been derived from CT, MRI and 3-D echocardiography, each of these imaging modalities on their own may not offer the best 3-D visualization of complex congenital heart disease.
Through using integrated, or hybrid 3-D imaging, Vettukattil said this can combine the strengths of multiple modalities for an enhanced 3-D model of complex congenital heart disease.
In the 2016 article, 3-D transesophageal echocardiogram (3DTEE) combined with CT imaging of a patient with L-TGA, VSD and pulmonary atresia were shown to be of adequate quality to perform hybrid 3-D printing of the heart, demonstrating the feasibility of the technique.
Along with helping interventional cardiologists better plan and customize surgery or device placement, hybrid 3-D printing also has the potential to help medical students and others in the field better understand complex congenital heart disease.
Katie Caron is an editor at Scranton Gillette Communications with B2B experience across industries including medical, home furnishings, water and infrastructure.
Reference:
1. Integration of Computed Tomography and 3-D Echocardiography for Hybrid 3-D Printing in Congenital Heart Disease. J Digit Imaging. 2016 Dec; 29(6): 665–669.




 February 13, 2026
February 13, 2026 









