Today's CT technology offers the key elements desired in a one-stop-shop cardiac imaging modality. These include good anatomical imaging to identify possible blockages, functional data via perfusion imaging, clear image datasets to plan and guide interventions, and data to back its prognostic value. This was according to James Min, M.D., FACC, New York Presbyterian, who spoke at several sessions on CCTA at the American College of Cardiology (ACC) 2015 meeting. He said the introduction of 64-slice CT systems since 2005 has made coronary CT angiography a widespread viable imaging option. The high level of radiation dose associated with older scanners (about 30 mSv in 2005) has dropped precipitately in recent years with the introduction of new scanner technology, iterative image reconstruction software and other technical changes in how scans are performed. Today, Min said routine cardiac CT scans can be performed at or below 1 mSv.
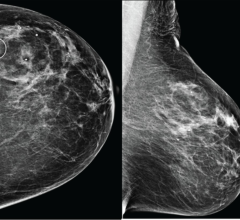
"Once you hit that 1 mSv or less range, you are hitting the area that is equal in dose to a screening mammogram," Min explained.
He stressed the clinical data from numerous randomized trials showing how CCTA can be a reliable first-line gatekeeper to the cath lab. He said CT perfusion imaging (the assessment of iodine contrast media in the myocardium as a surrogate measure for blood flow) can show areas of ischemia, similar to nuclear myocardial perfusion scans.
Since 2007, studies have validated the use of CT perfusion, said Ricardo Cury, M.D., FAHA, FSCCT, FACC, chairman of radiology, director of cardiac imaging, Baptist Health of South Florida, Miami Cardiac and Vascular Institute. He said there are now about 50 single-center studies comparing CT perfusion to other commonly used function testing modalities, including nuclear imaging, angiography, SPECT myocardial perfusion, angiography with invasive catheter fractional flow reserve (FFR) and MRI. In the past few years there have been some large retrospective meta analysis studies for the use of CT perfusion and two major multi-center, randomized trials.[1, 2]
"The evidence is there. If you have more than 50 studies showing CT perfusion is equivalent with other modalities and two large scale studies showing you are adding incremental value to CCTA, it becomes a question of how to implement this into clinical practice," Cury said. "In all these studies, CT perfusion is comparable to nuclear myocardial perfusion imaging. We showed it is at least equal to SPECT myocardial perfusion scans."
Performing CT Perfusion Scans
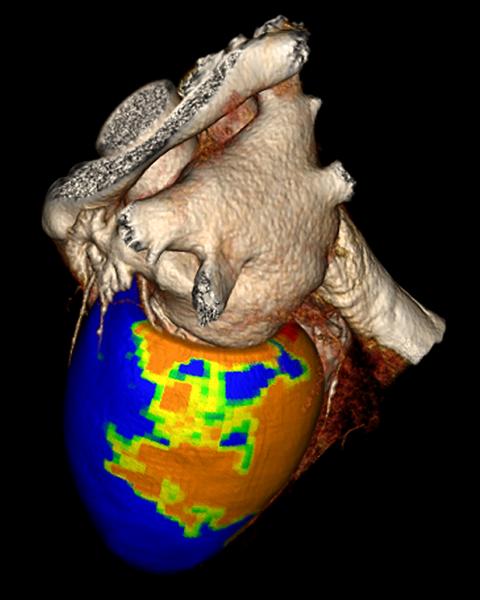
On a basic level, Min said experienced cardiac CT readers should be able to identify perfusion defects (dark areas of the myocardium devoid of contrast due to the lack of blood flow) quickly on first pass CT scans. He said the more advanced method is the "sit and spin" approach, where the scanner makes numerous rotations to visualize the wash in and wash out of contrast in the myocardium. CT perfusion software can help enhance visualization and enable quantification.
Cury said a coronary CCTA scan is always performed first, and then a separate perfusion scan using rest and pharmacological stress protocols is performed. The two scans take a total of about 30 minutes to perform.
Adoption of CT Perfusion
"At this point, we are having early adopters of CT perfusion in clinical practice," Cury said. Most of these adopters are experienced CCTA centers that are integrating perfusion as part of their daily routine, or centers using it for clinical studies. He said it will likely be another five years or so before CT perfusion is used for standard cardiac imaging at other centers.
The biggest driver for its adoption will likely come from healthcare reform, which will convert the U.S. healthcare system from a fee-for-service model to a value-based payment system, Cury said. CT perfusion is another step toward making CT a less expensive, one-stop-shop for cardiac imaging without the need for other tests, overnight admissions or unnecessary diagnostic catheterizations.
"Economics play a big role. As healthcare changes to a value-based system, CT perfusion will become very attractive," Cury explained. "It's very convenient from a patient's perspective because if they have an intermediate lesion seen on a scan, with CT perfusion you can see its impact right on the spot," Cury said. "In the past you had to send the patient for a nuclear scan the next day."
Perfusion Analysis Software
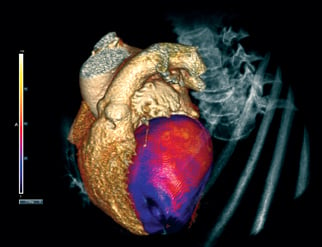
All the major CT vendors and the third-party advanced visualization vendors Vital and TeraRecon offer CT perfusion analysis software. They all operate on the same principle of measuring the Hounsfield units associated with iodine contrast mixed in the blood and tracking and mapping its levels in the myocardium throughout the cardiac cycle. The software can then create color-coded perfusion maps on 3-D reconstructions, multi-planar views or on bull's eye maps. These systems also offer quantification of the contrast levels in the tissue.
"For an experienced reader, you don't need software, you can process the images in your mind based on the gray levels of contrast in the tissue," Cury said. "You can detect if there is an ischemic defect and if it is reversible."
However, he said the software allows for automated quantification and helps verify the reader's qualitative assessment of the images.
"I think it is very promising and in specific settings it might be able to replace nuclear myocardial perfusion imaging," Cury said.
He said it is ideal for patients who present to the emergency department with chest pain, because it offers an immediate assessment of perfusion without the wait or need for overnight admission to undergo a nuclear scan in the morning, or a diagnostic angiogram.
FFR-CT and a New Perfusion Paradigm
Min said the next major step in CT perfusion imaging is the use of FFR-CT, which gained U.S. Food and Drug Administration (FDA) approval in November 2014. Catheter-based, invasive FFR is considered the gold standard to determine if coronary lesions are hemodynamically significant and require stenting. The FDA cleared the noninvasive, virtual FFR-CT software based on its close correlation with invasive FFR.
Using computational fluid dynamics supercomputing analysis software, FFR-CT technology solves millions of complex equations simulating blood flow in the coronary arteries to provide a mathematically derived FFR. The software (offered by Heart Flow Inc.) creates a virtual 3-D model of the patient's coronary tree. It goes beyond the perfusion data included in the CT dataset or in an invasive FFR for a single lesion to show FFR readings for the entire coronary tree. This includes cumulative measures for segments with long diffuse lesions and the impact of multiple lesions in a vessel branch. The FFR-CT color-coded coronary tree showing various FFR values overlaid on a 3-D reconstruction of the patient's heart to show the associated anatomical landmarks, which can be used for orientation during interventional revascularization procedures.
Results of the FFR-CT
RIPCORD study, presented at the EuroPCR 2015 in May, showed the technology might help change the course of treatment in more than one-third of patients with coronary artery disease. In the study, three experienced cardiologists reviewed CCTAs of 200 consecutive cases of patients with stable chest pain. The physicians agreed upon a plan to manage each patient: optimal medical therapy, a percutaneous coronary intervention (PCI) or coronary bypass surgery. In some cases, the physicians agreed that they were unable to make a decision and needed more information, such as an invasive diagnostic angiogram with associated invasive FFR. Next, the physicians were shown the results of the FFR-CT analysis for each case and made a second management decision incorporating these data. Overall, the management plan was changed in 72 of the 200 patients (36 percent). In 16 of the 87 cases considered candidates for PCI based on the angiogram (18 percent), one or more of the target lesions was changed using the FFR-CT analysis.
"FFR-CT has a lot of promise and I believe in the technology," Cury said.
However, as with any medical technology, Cury said it has advantages and disadvantages. FFR-CT does not require a second scan or the administration of adenosine or other pharmacological stress agents. It also provides FFR data without the need to send a patient to the cath lab. He said the downside of the technology is that hospitals need to send patient data to a third-party for analysis and it requires up to a 24-hour turnaround time for the FFR-CT report. Another issue is that the technology has an issue processing CT scans in patients with high levels of arterial calcium burden, where the lumen is difficult to define.
For these reasons, Cury said CT perfusion will likely be used as a first line option by many centers until FFR-CT analysis technology can be enabled at the centers themselves and the image processing time reduced to a few hours, rather than an entire day.
References:
1. Cury RC, Kitt TM, Feaheny K, Blankstein R, Ghoshhajra BB, Budoff MJ, Leipsic J, Min JK, Akin J, George RT. "A randomized, multicenter, multivendor study of myocardial perfusion imaging ith regadenoson CT perfusion vs single photon emission CT." J Cardiovasc Comput Tomogr. 2015 Mar-Apr;9(2):103-12.e1-2. doi: 10.1016/j.jcct.2015.01.002. Epub 2015 Jan 7. PubMed PMID: 25726411.
2. Rochitte CE1, George RT, Chen MY, et al. "Computed tomography angiography and perfusion to assess coronary artery stenosis causing perfusion defects by single photon emission computed tomography: the CORE320 study." Eur Heart J. 2014 May;35(17):1120-30. doi: 10.1093/eurheartj/eht488. Epub 2013 Nov 19.


 February 06, 2026
February 06, 2026