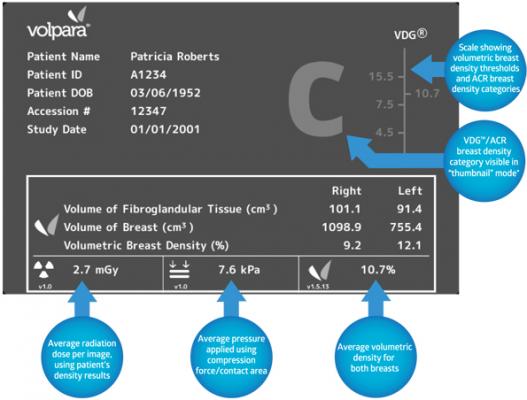
Image courtesy of Volpara
January 8, 2015 — The value of volumetric breast density to help improve breast cancer risk prediction models and monitor clinical treatment was the focus of numerous abstracts presented at the 2014 San Antonio Breast Cancer Symposium (SABCS). Five scientific abstracts highlight the use of VolparaDensity automated breast density software to provide insight into the impact of temporal changes of breast density, utilize volumetric density to improve breast cancer risk prediction to support personalized screening models and monitor the effectiveness of chemo-preventive treatments.
In the study, “Volumetric breast density improves breast cancer risk prediction”, researchers from University of Virginia Health System evaluated the association between risk factors and breast cancer diagnosis. The study enrolled 3,445 women in 839 cases with 2,606 controls. A multivariate analysis was conducted using 860 cases and 1,683 controls. Risk factor information was collected using a self-reported electronic questionnaire and mean automated volumetric breast density from VolparaDensity was calculated for each patient as a percentage. Results of the study demonstrate that the addition of volumetric breast density improved breast cancer risk discrimination, which is critical in model development if screening recommendations are to be individualized. The risk model used automated measurement of breast density as a continuous variable that proved to be one of the top five predictors of breast cancer risk in the study population. Volumetric breast density demonstrated improved discrimination for both the full prediction model (0.86) and a minimal model (0.82) (13 covariates) compared with the Tyrer-Cuzick (IBIS) model (0.74).
University of Virginia researchers also presented the results of the “Association of mammographic density and molecular breast cancer subtype”. This study looked at the association of mammographic density measured by VolparaDensity and molecular subtypes of breast cancer. Visual BI-RADS density scores and volumetric breast density measurements were obtained for 457 patients with invasive breast cancer. Molecular subtypes (Luminal A, Luminal B, Her-2-Neu and Triple Negative) were categorized according to hormone receptor status (i.e. estrogen receptor (ER), progesterone receptor (PR) and Her-2 receptor), tumor grade and mitotic score. After adjusting for age, race, BMI, family history of breast cancer and lobular carcinoma in situ (LCIS), volumetric breast density was significantly associated with Her-2-neu positive tumors (p = 0.035). A similar analysis showed that this association was not seen for visual BI-RADS categories (p = 0.671 and p = 0.099 for BI-RADS 3 and 4, respectively). The results show that women with denser breasts by continuous-scaled quantitative measurements are at higher risk for Her-2+ tumors; an association not delineated using standard BI-RADS density classification. The identification of risk factors that are associated with specific breast cancer subtypes could help to inform personalized risk prediction models and prevention strategies.
Results of the IBIS-I Prevention Trial demonstrated that tamoxifen prevented breast cancer in women with greater than 9% absolute reduction in visually assessed mammographic density. In the study, “Predicting the effect of tamoxifen on the breast: Change in measures of breast density, serum markers and SNPs” University of Manchester researchers compared the effect of tamoxifen on mammographic density and in a different patient population using several methods (Quantitative visual to the nearest 5%, visual analogue scale (VAS), Cumulus, Volpara and Quantra). The results from the original IBIS-I reader were reproducible in this new population of women; however, other readers using VAS detected fewer changes in mammographic density, suggesting a difficulty in detecting change in general radiological practice. The results indicated that 72% and 68% of women experienced greater than 10% change in dense volume using Volpara and Quantra, respectively, after tamoxifen treatment. Women who experienced less than 10% change in mammographic density were more likely to have increased triglycerides after tamoxifen treatment, suggesting that triglycerides could be used as a surrogate marker for mammographic density change. While Cumulus was able to detect changes in mammographic density, it is difficult to implement clinically, and automated measures of dense volume are likely to be the most useful.
The study “Effects of statin use on volumetric mammographic density: Results from the Karolinska mammography project for risk prediction of breast cancer (KARMA) study” looked at the association of volumetric breast density, statin use and hormone replacement therapy (HRT) use. Results suggest that volumetric breast density percent was significantly lower in statin users, although the corresponding higher non-dense volume in statin users explained this association. Overall, no difference in absolute dense volume (cm3) was observed between statin users and non-users. However, among women who had reported ever using HRT, a significantly larger absolute dense volume was observed for statin users versus non-users (p=0.03). HRT use potentially modifies the effect of statins on mammographic density, and this relationship requires further investigation in the context of breast cancer risk.
High mammographic density (MD) in women is strongly associated with breast cancer risk. However, the structural and compositional differences between dense and non-dense breast tissues are not well defined. University of Manchester researchers investigated the relationship between mammographic density, collagen deposition and fibril alignment and tissue micro-stiffness, in similarly aged individuals without adjacent cancer in the study “High mammographic density is associated with deposition of organized fibrillar collagen and increased stiffness in periductal breast stroma”. Researchers used Volpara to measure volumetric density in 22 women (54-66 years) undergoing risk-reducing surgery or mastectomy. Localized regions of elevated density determined from digital mammograms, were isolated from patients of low and high overall density. All elevated-density regions contained considerable amounts of stromal connective tissue. However, there were significant differences in these regions from women with low versus high overall mammographic density. High density is a significant risk factor for breast cancer, yet its molecular determinants in the normal, non-cancerous breast are poorly defined. The results suggest that high density is associated with more organized fibrillar collagen, leading to increased stiffness of the periductal breast stroma, which may contribute to cancer onset.
Ralph Highnam, Ph.D., Volpara Solutions’ CEO and Chief Scientist comments: “With consistent and accurate volumetric measurements of breast composition that are strongly validated to breast MRI, we now are beginning to develop an understanding, as never before, of patient risk profiles and the underlying biology of the breast. As evidenced by the presentations at the San Antonio Breast Cancer Symposium, that understanding is leading to a new range of clinical research into the impact of temporal changes of density, development of risk models for personalized screening protocols as well as monitoring the effectiveness of tamoxifen and other chemo-preventatives that could have tremendous impact on the prevention, detection and treatment of breast cancer.”
For a complete summary of the volumetric research presented at SABCS: www.volparasolutions.com/Dejavu/wp-content/uploads/2014/12/SABCS-2014-R…
For more information: www.volparasolutions.com


 February 17, 2026
February 17, 2026 









