
Siemens' MAMMOMAT Novation S is designed for facilities transitioning to digital breast imaging without needing advanced diagnostic functionality.
The tide may finally be turning in the fight against cancer as the decline in cancer deaths nearly doubled from 2002 to 2004, the American Cancer Society reported in October 2007.1 Early diagnosis enabled by digital mammography and breast MRI are currently building the momentum, but new developments in tomosynthesis, cone-beam CT and biomarkers may be the tipping point.
Although mammography rates dropped four percent in 2005 from a high of 70 percent in 2000,2 and there is concern that women will be detected with a later stage of cancer, manufacturers continue to step-up to the fight against breast cancer with novel solutions and techniques for early diagnosis — the approach clinicians hope will continue turning the tide.
Mammography answers the screening call
When Fuji released the FCRm in 2006, healthcare centers had a lower-cost digital imaging alternative to full-field digital mammography (FFDM). It didn’t take long for FFDM manufacturers to respond. At RSNA 2006, Hologic, Philips Medical Systems and Siemens Medical Solutions introduced a mammography system optimized for screening.
Siemens’ MAMMOMAT Novation S is designed for facilities that do not have the need for advanced diagnostic functionality or operate screening-only satellite centers. It uses an amorphous Selenium (aSe) detector, Siemens’ dose technologies, OpComp and OpDose, and comes standard with the Acquisition Workstation (AWS).
The works-in-progress MammoDiagnost DR from Philips combines automated reporting with Philips’ Xiris RIS and patient administration tools to enable high patient volumes. “Our Eleva workflow and new detector design allow a throughput of 10 patients per hour,” said Christiane Harms, product marketing manager, Mammography. “All movements and X-ray parameters are automatically set, plus prior images are pre-loaded to further streamline workflow, enabling the radiographer to concentrate on the patient.”
Hologic’s Selenia S, offered at a lower price point than the Selenia system, is optimized for screening mammography, satellite offices or mobile environments. Selenia S can be upgraded to include all diagnostic tools found on Selenia.
Also showcased in Hologic’s booth at RSNA was a new tungsten X-ray tube Selenia system. While the radiation exposures in digital mammography are already very low relative to the patient benefit in terms of early detection of breast cancer, Hologic is now offering a tungsten X-ray tube with rhodium and silver filters Selenia system. The use of a tungsten X-ray tube allows for dose reductions on the order of 30
percent, while maintaining the image quality already achieved with Selenia. The new system also offers the performance for some of the advanced applications under development, such as digital breast tomosynthesis, iodinated contrast and dual-energy breast imaging.
Tomosynthesis – waiting for FDA approval
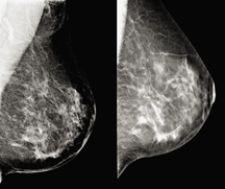
Because lower recall rates have high clinical significance and there is a corresponding reduction in the number of negative biopsies, technology that supports full-field digital mammography (FFDM) in reducing rates could prove extremely beneficial to clinician and patient alike.
Presented in the RSNA late breaking multicenter trial track were results from the first major multicenter study of digital breast tomosynthesis (DBT). According to lead author Elizabeth Rafferty, M.D., associate director of Breast Imaging at Massachusetts General Hospital, ROC analysis of 12 readers demonstrated statistically significant better performance in reading DBT with FFDM mammograms than FFDM alone.
“Across the spectrum of age and experience, every reader performed better,” noted Dr. Rafferty during Hologic’s RSNA Investor briefing. She estimates that tomosynthesis can reduce the screening recall rate in a normal screening population by 40 percent. “That is because tomosynthesis gives you the value of being able to correctly dismiss summation shadow or overlapping structures, more accurately characterize lesions and still see calcifications.”
Hologic is waiting for FDA approval of DBT and believes that breast tomosynthesis could become clinically available as early as mid-2008.
In other breast tomosynthesis news, Dexela Ltd. was recently awarded a GBP360,000 grant by the Technology Strategy Board, a business-led executive nondepartmental public body established by the UK government, to develop a second-generation DBT device in conjunction with two leading research universities, Oxford and UCL.
Breast MRI breaks new ground
Thanks in part to the American Cancer Society’s new recommendation for annual MRI exams in addition to mammography for patients deemed high risk for breast cancer, expect breast MR procedures to continue a significant growth path. According to Gail Prochaska, vice president, IMV Limited (Des Plaines, IL), breast MRI procedures grew 58 percent between 2003 and 2006.
Riding this wave, Aurora Imaging Technology rolled out the 1.5T Dedicated Breast MRI System with Bilateral 3D SpiralRODEO, a fully integrated MRI system designed specifically for breast imaging, creating an elliptical, homogenous field of view, providing coverage of both breasts, chest wall and axillae in a single bilateral scan. The breast MRI system can accommodate core biopsy or vacuum-assisted biopsy devices.
GE Healthcare also introduced Signa Vibrant, a dedicated 1.5T breast MR scanner. Signa Vibrant boasts several applications specifically designed for breast MR, including: VIBRANT acquisition, BREASE spectroscopy, integrated CADstream by Confirma and either GE’s High-Density 8-Channel Breast Coil or the Vanguard System by Sentinelle Medical, Toronto, a dedicated breast MR patient table with Variable Coil Geometry (VCG) for optimal positioning of coil elements. With a unique detachable table design, Signa Vibrant users can offer a more patient-friendly environment and reportedly achieve significant productivity benefits by preparing the next patient outside the exam room on a second table.
Addressing breast density
The ARIA Breast Imaging System (BIS) uses real-time through-wave ultrasound imaging with holography to create 3D images of the breast. The technology penetrates dense tissue with a high spatial and contrast resolution. In a preliminary report of a study conducted at Kadlec Medical Center (Richland, WA) and released by the company at RSNA, the investigators found that the ARIA BIS facilitated “detection of multifocal, nonpalpable and mammographically occult lesions.”
In their R2 computer-aided detection product area, Hologic previewed the works-in-progress Quantra, a fully automated tool that can help assess breast density. According to Julian Marshall, director of Product Management and principal engineer, computed-aided detection, Quantra creates a model of the X-ray imaging chain to calculate the type of breast tissue, including density, penetrated at each pixel in the image. “The technology automates measurement of the total volume of both breast and fibroglandular tissue,” explained Marshall. Hologic is beginning clinical trials to determine if the volume of fibroglandular tissue provides a more accurate assessment of the correlation between breast density and a woman’s future risk of developing breast cancer than the current standard of calculating total percentage of breast density.
Could cone-beam CT replace mammography?
Another technology that’s providing a clearer read on overlapping tissue is Cone- Beam CT. Researchers believe that cone-beam CT may potentially be used to replace mammography in screening and diagnostic breast imaging as cone-beam breast CT provides exceptional tissue contrast and can potentially reduce examination time with comparable radiation dose to conventional 2D mammography, according to a new study by a team of researchers from the University of Texas
MD Anderson Cancer Center in Houston.
The researchers used the cone-beam breast CT with its large area X-ray beam with a flat panel X-ray detector to scan and generate 3D images of the breast. The researchers placed the scanner below a table so that only the breast was exposed to radiation. This adjustment improved image quality and reduced radiation exposure. A complete rotation of the gantry around the breast was completed in less than one minute.
Findings from the study indicated that structured noise on cone-beam CT was minimal due to absence of overlapping tissue. Further, researchers found that breast anatomy was resolved on all images as skin, adipose, glandular regions, and that microcalcifications within cancers were clear. Additionally, because there was a lack of overlapping glandular tissue, detection of cancers based on morphologic assessment of tissue structures could be better compared with mammography.
In the pipeline
A new biomarker may have the potential to help mammography identify malignant versus benign breast lesions. RECAF (Receptor of Alpha Fetoprotein) has been found in over 90 percent of the breast cancers studied to date, according to BioCurex. The marker is present on the surface and within cancer cells, as well as in the blood of cancer patients.
According to the researcher who discovered the RECAF marker, Ricardo Moro-Vidal, M.D., CEO and president, the company is gearing up to begin a clinical trial with a leading institution to determine if a blood test can help radiologists better anticipate if a lesion is benign or malignant. In a malignant tumor, the levels of RECAF circulation within the blood increase. “If we can obtain 93 percent sensitivity and specificity, then we can potentially help reduce the number of false positives that lead to unnecessary breast biopsies,” he said.
1. Annual Report to the Nation on the Status of Cancer, 1975-2004, Featuring Cancer in American Indians and Alaska Natives." Published online Oct. 15, 2007, in Cancer. First author: David K. Espey, MD, Centers for Disease Control and Prevention.
2. Reported Drop in Mammography: Is This Cause for Concern?" Published online May 14, 2007, in Cancer. First author: Nancy Breen, PhD, National Cancer Institute


 January 19, 2026
January 19, 2026 









