WEBINAR: Myocardial CT Perfusion: A Comprehensive Appraisal of Patient Selection and Technique in a Multimodality Imaging Environment
Webinar Co-sponsored by SCCT and DAIC, supported by an educational grant from Canon Medical Systems USA
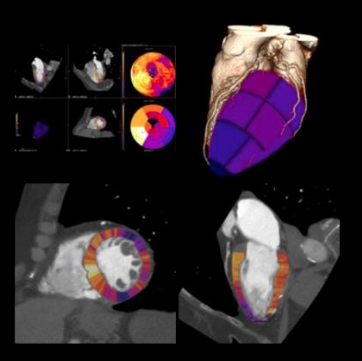
Chest pain is one of the most frequent reasons for an evaluation in the emergency room.There are multiple imaging modalities available to evaluate the patient with chest discomfort.This webinar aims at evaluating the role of myocardial CT perfusion testing in the patient with chest pain. The webinar will discuss patient selection, basic physiology, technique, test characteristics and case presentations at the end.
This webinar is co-sponsored by DAIC and the Society of Cardiovascular Computed Tomography (SCCT), and supported by an educational grant from Canon Medical Systems USA.
This is the first webinar in a two-part series. You can view the second webinar, Cardiovascular CT in pediatric patients: Technique and Applications With Emphasis on New Generation Scanners, can be viewed here.
Register for the on-demand version of this webinar
Learning objectives:
- To select the appropriate patient for CT Perfusion
- Understand the basic concepts/Physiology behind CT perfusion
- Discuss various protocols for the acquisition of CTP
- Understand the differences between static and dynamic CT perfusion
- Understand test Characteristics of CTP
The outline of the presentation as follows:
- Introduction
- CT Perfusion Physiology
- CT perfusion basics/Patient preparation
- CT perfusion protocols for rest/stress
- CT perfusion image acquisition
- CT perfusion post processing
- CT perfusion case presentations
Speaker:
 Ron Jacob, M.D., FACC, FASE, FSCCT, FSCMR, Director of Cardiac Magnetic Resonance Imaging, Lancaster General Hospital/PENN Medicine
Ron Jacob, M.D., FACC, FASE, FSCCT, FSCMR, Director of Cardiac Magnetic Resonance Imaging, Lancaster General Hospital/PENN Medicine
Jacob is the director of cardiac magnetic resonance imaging at Lancaster General Hospital/PENN Medicine. He has served on the International Outreach Committee of the Society of Cardiovascular Magnetic Resonance (SCMR) both as co-chair and most recently as chairman over the last two years. He has taught and helped to organize courses around the world focusing on the increasing the utilization of cardiac MRI and on the use of multimodality imaging in cardiovascular disease. Since he started in his current position, Lancaster General Hospital has participated in various research studies focusing on imaging, including the PROMISE study, RESCUE study, ACRIN PA 4008. He was invited faculty at the CT perfusion course conducted in Johns Hopkins and completed a pilot project using CT perfusion at Lancaster General Health/PENN Medicine. A new project evaluating the utility CT perfusion and CT-FFR is being started in 2019 at Lancaster General Health/PENN Medicine.
Intended Audience:
This activity is intended for radiologists and cardiologists involved in CT Perfusion and CT Scanners.
Register for the on-demand version of this webinar


 July 25, 2024
July 25, 2024