Nov. 13, 2014 — A new study by clinicians and researchers from Toronto and Vancouver, Canada, found that psychiatric patients who underwent SPECT-influenced treatments improved significantly more than patients who did not.
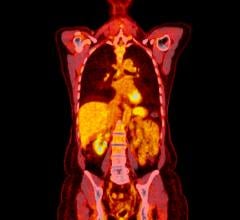
Published in the Journal of Neuropsychiatry, the study used SPECT imaging – Single Photon Emission Computed Tomography that measures blood flow and shows over-activity, under-activity or non-activity in the brain. The research shows that SPECT imaging is a potentially helpful tool to gain more information on patients who struggle with mental health issues and thus better target their treatment.
Daniel Amen, M.D., Founder of Amen Clinics who is not related to the research says, "This study points to a significant advancement in the care of people who suffer with mental health issues. Until now, standard diagnoses in psychiatry are made primarily through talking to patients and looking at symptom clusters without any biological information. Psychiatry is the only medical specialty that virtually never looks at the organ it treats. It is a major step forward."
Researchers and clinicians have debated the clinical benefits of SPECT for decades, but ongoing new research consistently is showing its value in clinical practice.
The clinicians involved in the study have been using SPECT in clinical practice for nearly a decade and have recruited other physicians in Canada to do the same. There are a number of clinics in the United States, Japan and Chili who use SPECT on a regular basis.
Results from Toronto and Vancouver, Canada study not only support SPECT imaging science in treating patients for improved outcomes, but also aids the debate – supporting that SPECT is a groundbreaking tool that should be used in treatment of mental healthf.
For more information: hneuro.psychiatryonline.org


 February 03, 2026
February 03, 2026