Turning 40 is a benchmark birthday for many women in the United States. While a pessimist might view it as a signal that their glory days are over, more and more women are optimistic about the milestone, seeing it as a kickoff into the best years of their lives. But one thing is true for all women – health needs and preventative wellness routines should begin to change at age 40.
“For some women, they have health history or specific reasons to begin mammography before age 40. But for the average woman who has never had a breast screening, we recommend she begin a routine annual wellness mammogram, starting at age 40,” said Dr. Stephen Rose, chief medical officer, Solis Mammography. “Simply put, women in their 40s have the most to gain from being proactive about early detection. Major studies have shown time and again that in addition to saving lives, early detection offers greater quality of life as treatment at earlier stages is less invasive and less costly.”
Solis Mammography is expected to complete nearly 1 million procedures in 2018. Making them the nation’s largest independent provider of breast screening services. With this, Solis Mammography has some of the nation’s most comprehensive research data supporting its claim that women should begin annual mammography starting at age 40. This is in contrast to some confusing and conflicting advice from various media and non-physician-led organizations.
“While it’s true that breast cancer treatment has come a long way in recent years, this should in no way deter a woman from participating in the benefits of annual mammography,” said Solis Mammography CEO James Polfreman. “The fact is that cell growth replicates at a faster rate in younger tissue. So, the younger you are, the more important it is to find any anomaly earlier. Research and technological advances in mammography have led to an all-time high in survival rates from breast cancer diagnosis. This tells us we’re on the right path, and annual mammography is a key part of that success story.”
Four compelling reasons to begin annual mammograms at 40
The numbers. According to the American Cancer Society, 20 percent of all breast cancers are found in women under 50. If the cancer is found early, in what is known as stage zero or stage one, the five-year survival rate is nearly 100 percent. Simply stated, early detection is the closest thing to a cure, and mastectomies are no longer the first line of defense.
Women in their 40s have the most to gain. “Today’s high-quality screenings benefit 40-year-old women the most,” explained Dr. Rose, a radiologist with more than 25 years in the field of breast screening specialization, involved in several published national studies. “Advancements like 3-D mammography (digital breast tomosynthesis), and breast specialization have a significant impact on the quality of the mammography result. Today, we know one mammogram isn’t the same as another. It’s important to know what to look for in your provider to ensure the most accurate results.”
A chance for women to take charge of their health. Conflicting recommendations from some non-physician led organizations have suggested a “reasonable trade-off” to the “fear, anxiety and stress” of a “false positive” (otherwise known as a recall for additional images) is to delay annual screenings for five to 10 critical years. This advice encourages a foolhardy “Russian Roulette” approach to monitoring breast health. It suggests no alternative to mammography; instead suggesting screenings be ignored entirely. The studies and clinical evidence are clear. Early detection provides women with the greatest opportunity for long-term survival and quality of life through the least invasive treatment when caught at the earliest possible stage.
Treatment is an option; knowledge is not. Instead of focusing on overdiagnosis as the problem, the real question at hand is overtreatment. With the advancement of medicine and less invasive treatments, women have more options for success. And in some cases, patients may opt not to treat at all, rather to monitor changes over time. These are discussions a woman can and should have with her doctor AFTER getting all the facts. Avoiding the facts is not a solution.
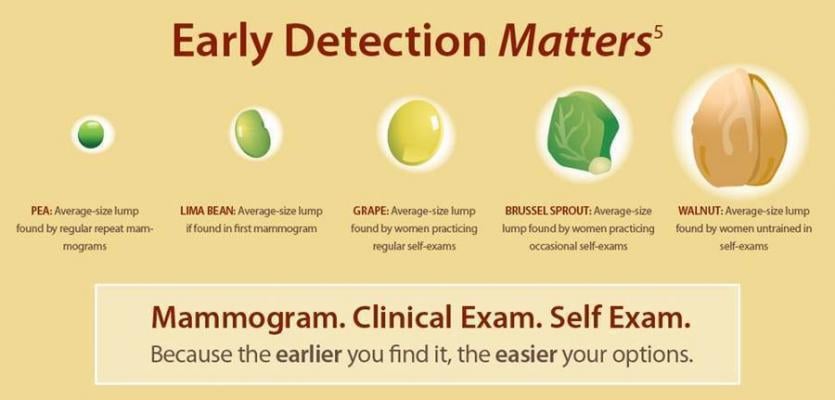
Pea versus walnut: Why mammograms help with early detection
Dr. Rose suggests thinking of a pea versus a walnut, when considering why early detection is so important. The average size of a lump found in a woman who gets regular annual mammograms is the size of a pea. The size of a lump found by a woman who does only occasional self-exams is the size of a walnut.
“Imagine the difference in treating the pea versus the walnut. It’s the pea that gives us our best options for treatment,” Dr. Rose advised. “Put simply, the larger the lump, the more invasive and costly the treatment options become, and the more risk that is associated with long-term outcomes.”
For more information: www.SolisMammo.com


 February 18, 2026
February 18, 2026 









