Getty Images
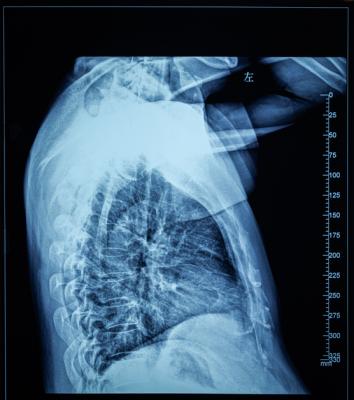
April 30, 2021 — For many patients with localized lung cancer (non-small-cell lung carcinoma and small cell lung carcinoma), high-dose radiation with concurrent chemotherapy is a potential cure. Yet this treatment can cause severe, acute inflammation of the esophagus (esophagitis) in about one in five patients, requiring hospitalization and placement of a feeding tube.
A team of radiation oncologists at Mass General Cancer Center demonstrate in an early clinical trial that the radiation beam can be carefully "sculpted" to deliver the majority of a radiation dose directly to the tumor while effectively sparing tissues in the side of the esophagus away from the affected lung (the contralateral esophagus), thereby limiting inflammation and preserving swallowing function.
The researchers describe their contralateral esophagus sparing technique (CEST) in a study published in JAMA Oncology.
"Severe grade 3 esophagitis is a terrible complication of radiation and chemotherapy," said co-senior author Henning Willers, M.D., director of the Thoracic Radiation Oncology Program at Mass General Cancer Center. "It happens 5% to 10% of the time in patients with non-small-cell lung cancer, and 15% to 20% of the time in patients with small-cell lung cancer. Even grade 2 esophagitis, one step lower in severity, can be really tough, with patients requiring narcotics for many weeks to cope with the pain," he said.
Starting in 2013, Willers and colleagues carefully observed outcomes with various treatment techniques, including radiation methods used to treat head and neck and prostate cancers, and using a method of radiation delivery called intensity-modulated radiation therapy (IMRT) they devised CEST.
The technique involves imaging the esophagus and then shaping a high-dose radiation beam so that the maximal amount of radiation energy is delivered to the tumor, with a steep dropoff in energy across the esophagus, thereby sparing as much as possible the normal tissues and function in the side of the esophagus farthest away from the treatment site.
In their initial clinical experience, investigators saw that among patients with locally advanced lung cancers who were treated with CEST and chemotherapy, none had grade 3 or greater esophagitis, and only about 20% had grade 2 esophagitis, which was relatively mild, despite the fact that these patients had received high doses of radiation.
"In 2014, when I was a radiation oncology resident, I noticed that patients did really, really well with our use of this sparing technique, and with Christine C. Olsen, M.D., co-principal investigator of the trial, we moved to test this concept on a formal clinical study," says lead author Sophia C. Kamran, M.D., now a staff radiation oncologist at the Cancer Center.
To better determine the frequency of esophagitis in patients treated with CEST, the investigators designed a phase 1 trial with 27 patients, 25 of whom completed combined chemotherapy and radiation. Of this group, ranging from 51 to 81 years of age, 19 had non-small-cell lung cancer, and 6 had small-cell lung cancer.
None of the 25 patients who completed chemoradiation developed grade 3 esophagitis, while 7 experienced grade 2 esophagitis. Other treatment side effects were within the range of what can be expected for this type of cancer. Two-thirds of patients remained alive at two years after chemoradiation, and none had an isolated local tumor recurrence.
"Our findings support emerging national guidelines, which are increasingly recognizing the importance of sparing the esophagus, although an effective method to do so has neither been formalized nor well defined until now. This is the first prospective trial reporting on the use of a formalized technique," said Kamran.
For more information: www.


 February 04, 2026
February 04, 2026 









