January 2, 2015 — A clinical trial that combined stereotactic body radiation therapy (SBRT) with a specific chemotherapy regimen more than doubled survival rates for certain stage 4 lung cancer patients, UT Southwestern Medical Center cancer researchers report.
The combination of the chemotherapy regimen erlotinib with SBRT improved overall survival time to 20 months compared to historic 6- to 9- month survival times among erlotinib-only treated patients. The combination improved progression-free survival — the time without the reappearance of cancer — from the historical two to four months to 14.7 months for similarly selected lung cancer patients.
“Our approach dramatically changed the pattern of relapse. We saw a shift in failure from existing, local sites to new, distant sites,” said senior author Robert Timmerman, M.D., director of the Annette Simmons Stereotactic Treatment Center and vice chairman of radiation oncology at UT Southwestern. “This shift resulted in a surprisingly long remission from the reappearance of cancer in treated patients.”
This Phase 2 clinical trial involved 24 patients with stage 4 non-small cell lung cancer (NSCLC) whose cancer has continued to spread during their initial therapy. Such patients typically have poor survival rates, and SBRT is not typically used in these patients, said first author Puneeth Iyengar, M.D., assistant professor and director of clinical research of radiation oncology, and co-leader of the Simmons Cancer Center Thoracic Oncology Group.
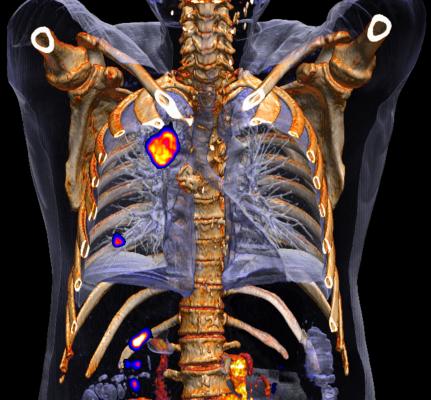
SBRT is a type of radiation therapy in which a few very high doses of radiation are delivered from multiple angles to small, well-defined tumors. The goal is to deliver a radiation dose high enough to kill the cancer while minimizing exposure to surrounding healthy tissue and organs, explained Timmerman.
SBRT has been shown to offer better cure rates in certain instances, particularly for cancers that have metastasized, said Timmerman.
The results are reported in the Journal of Clinical Oncology of the American Society of Clinical Oncology.
For more information: www.utsouthwestern.edu


 January 30, 2026
January 30, 2026 









