November 24, 2014 – Lung cancer patients with minimally invasive adenocarcinoma (MIA) have similar, positive five-year disease-free survival (DFS) and overall survival (OS) rates as patients with adenocarcinoma in-situ (AIS), according to research presented at the 2014 Chicago Multidisciplinary Symposium in
Thoracic Oncology.
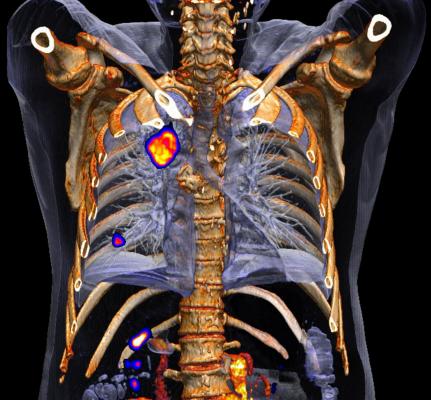
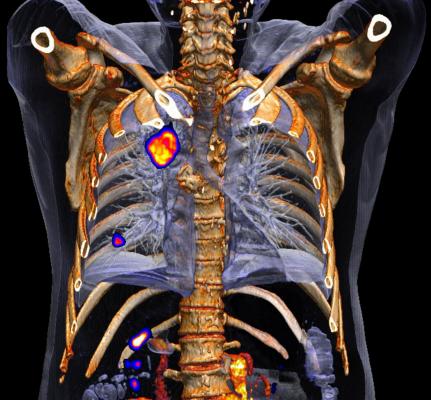
Lung adenocarcinoma accounts for 60% of all non-small cell lung cancers and is the most common form of
lung cancer in both smokers and non-smokers and patients younger than 45 years old. Bronchioloalveolar carcinoma is a type of adenocarcinoma that affects the cells lining the alveoli (small air sacs) of the lungs. Invasion occurs when the tumor extends beyond the alveolar lining and evokes a fibroblastic stromal response. These types of tumors, if =3 cm in size, are reclassified as AIS (no tumor invasion) or MIA (=0.5 cm of tumor invasion), according to the 2011 IASLC/American Thoracic Society /European Respiratory Society (IASLC/ATS/ERS) International Multidisciplinary Classification of Lung Adenocarcinoma. This study examines the difference in DFS and OS rates for patients with diseases classified as AIS and MIA and determines if it is beneficial to categorize tumors according to additional sub-types.
The study authors conducted a comprehensive search of studies published from 2011 to 2014 in the MEDLINE, Embase and Cochrane databases. Studies selected for analysis provided survival outcome data for at least eight cases classified as AIS or MIA based on the 2011 IASLC/ATS/ERS classification. Excluded studies did not report survival information. A systematic analysis of DFS and OS data was performed using the random effect model of the Comprehensive Meta Analysis (Version 2.2) software.
The study’s analysis included information from 18 clinical studies published from 2011 and 2014. The 18 studies included a total of 863 patients, with 451 patients classified as AIS and 344 patients classified as MIA. One study reported survival data on patients (68) with AIS and MIA grouped together. The median age of all patients was 67.5 years old. 61% of patients were female, and 43% of all patients were smokers. The median tumor size was 1.3 cm.
The five-year DFS and OS rates were not statistically different between patients with AIS and MIA. The five-year DFS rate was 97.7% for all patients included in the analysis. The five-year DFS rate was 97% in patients with AIS and 96.7% in patients with MIA (p=0.34). The five-year OS rate was 97.3% for all patients included in the analysis. The five-year OS rate was 97.5% in patients with AIS and 96% in patients with MIA (p=0.58).
“Some researchers have advocated that AIS and MIA should have separate categorization,” said lead author Madhusmita Behera, Ph.D., associate director of research in the Department of Hematology and Medical Oncology at Winship Cancer Institute of Emory University in Atlanta. “Our analysis demonstrates that these carcinomas, especially when the tumor is 3 cm or less in size, are associated with excellent survival outcomes; therefore, tumor sub-classification into AIS and MIA may not provide additional prognostic information.”
For more information: thoracicsymposium.org/