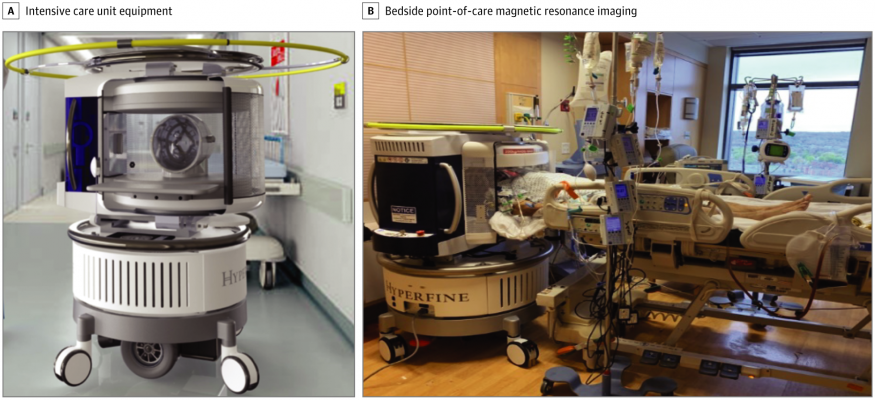
All intensive care unit equipment, including ventilators, pumps, and monitoring devices, as well as the point-of-care magnetic resonance image operator and bedside nurse, remained in the room. All equipment was operational during scanning. Image courtesy of JAMA Neurology
September 11, 2020 — A portable, low-field magnetic resonance imaging (MRI) device can be safely used at bedside in complex clinical care settings to evaluate critically-ill patients for suspected stroke, traumatic brain injury (TBI), or other neurological problems, results of a proof-of-concept study show.
"How can a portable low-field device that operates on a standard electrical plug change the paradigm? It can bring the MRI to the bedside, and it can do so in a hospital environment where there is metallic material nearby, and can do it safely because the magnetic field strength is lower," said W. Taylor Kimberly, M.D., Ph.D., chief of the division of Neurocritical Care at Massachusetts General Hospital (MGH).
Among 30 patients in a the Yale Neuroscience intensive care unit (ICU), the bedside MRI system produced important neuroimaging findings in 29, and the findings jibed with conventional radiology findings in all but one case, found Kimberly, Matthew S. Rosen, Ph.D., director of the Low Field MRI and Hyperpolarized Media Lab and co-Director of the Center for Machine Learning at the Athinoula A. Martinos Center for Biomedical Imaging at MGH, and colleagues at Yale University in New Haven, Connecticut.
In addition, the bedside MRI detected abnormal neurologic findings in eight of 20 patients with altered mental status in a COVID-19 ICU.
The investigators report their finding online in the journal JAMA Neurology.
MRI is unparalleled as an imaging technology for detecting disease or injury to the brain and central nervous system, but traditional MRI units are immobile behemoths containing large, heavy magnets made of super-conducting material that requires super-cooling with liquid nitrogen or helium. In addition, the high magnetic field strengths of standard MRI units - 1.5 to 3 Tesla - require careful screening of patients to ensure that there are no ferrous metals in or on their bodies (such as medical implants, insulin pumps, or shrapnel fragments) that could cause serious injury during imaging, and any medical equipment containing ferromagnetic components must be kept out of the MRI room.
In contrast, the mobile MRI system trades some of the high-resolution imaging quality of a fixed MRI for portability and lower cost. The device contains a 0.064 Tesla permanent magnet that does not require cooling, and can be plugged into a single 110 volt, 15 amp outlet, making it suitable for use in settings such as emergency departments, mobile stroke units, and regions with limited medical resources. The lower strength magnetic field does not interfere with metal-containing equipment in patient care units.
The system grew out of work Rosen began more than a decade ago at the request of the U.S. Department of Defense (DoD). DoD staff were concerned that soldiers with battlefield injuries might have shrapnel in their heads that could cause serious injury or death if they were placed into a high-field scanner.
"This is an enabling technology to bring non-invasive neuroimaging with the soft-tissue contrast and all of those things neurologists have been relying on for years to environments where it otherwise would not be possible," Rosen said.
For more information: http://www.


 February 04, 2026
February 04, 2026 









