March 30, 2020 — In the wake of the COVID-19 pandemic, a team of radiation oncologists from the U.S. and U.K. is recommending a new framework for making decisions about radiation therapy for prostate cancer patients that weighs risks and benefits during these difficult times.
The approach recommends protecting patients, care providers and society through increased use of telemedicine consultations, as well as avoiding, deferring and shortening radiotherapy to the safest extent possible.
“During the current crisis, delaying radiotherapy treatment — which requires patients with prostate cancer to make multiple visits for testing and treatment — reduces their risk of exposure as well as helping to protect members of their care team. And because COVID-19 is so highly infectious, this also helps to protect society as a whole,” said Daniel Spratt, M.D., co-chair of genitourinary clinical research at the University of Michigan Rogel Cancer Center and corresponding author of the recommendations. A pre-print of the recommendations was published online in Advances in Radiation Oncology.
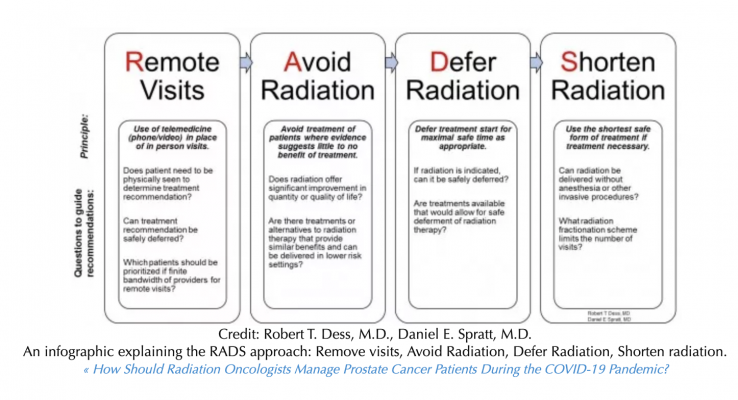
Spratt and Robert T. Dess, M.D., an assistant professor of radiation oncology at Michigan Medicine, developed a framework dubbed RADS — for Remote visits and Avoid, Delay, and Shorten radiotherapy. This framework, elaborated over the past week as COVID infections rose globally, is now being adopted and used by the National Institute for Health and Care Excellence (NICE) and NHS England (NHSE) in the United Kingdom, Spratt notes.
“As prostate cancer therapy has advanced, it has also become more complex, with increasing use of advanced imaging and other techniques that require extra procedures and visits, many of which require the use of masks, gloves and other types of protective equipment that are currently needed by frontline providers,” he added.
To come up with the new recommendations, the group analyzed national guidelines and systematic reviews, along with data from previous and ongoing clinical trials. The new guidelines are intended to apply only to patients who are not infected with COVID-19; those who have already tested positive should follow plans and procedures put in place at their local hospital, the team notes.
“We issued these recommendations assuming that the pandemic will last for at least several months, with multiple waves of varying length, and place new overall stress on hospital systems, along with causing disruptions to hospital staffing from illness, quarantine and family responsibilities,” Spratt said.
Compared to other types of cancer, many prostate cancer patients have a favorable prognosis and the risks caused by delaying radiation therapy for several months is low, the group found. For those with more aggressive forms of the disease, the use of hormone therapy can safely delay the start of treatment for several months.
“For these reasons, short delays in radiotherapy are almost always safe for prostate cancer,” Dess said. “For patients with more aggressive disease, extended delays should be avoided.”
Under RADS, the recommendations include:
- Remote visits should be used in place of in-person visits when patients don’t need to be seen physically to determine a course of treatment. The added value of a physical exam is usually outweighed by the risk of COVID-19 exposure.
- Avoid radiation when evidence suggests it would be of little or no benefit to a patient. Multiple clinical trials have shown favorable outcomes with a watchful approach to monitoring patients with low- to intermediate-risk cancers.
- Delay treatment for as long as possible, depending on each patient’s individual circumstances. If a patient’s disease is progressing rapidly, the benefits of treatment must be weighed against COVID-19 exposure and other potential risk factors, such as other chronic conditions the patient may already have.
- Shorten radiotherapy treatments to the shortest number that been shown to be safe and effective. This can help limit the number of visits each patient will need to make.
“The COVID-19 pandemic is presenting new challenges for providers who care for all types of cancer patients, and creating difficult decisions around providing the most beneficial care while managing the risks and strains on the health care system caused by the outbreak,” Spratt said. “Our goal was to quickly provide a framework based on the most up-to-date research to help guide treatment decisions for prostate cancer patients around the globe.”
Additional authors on the paper include: Nicholas G. Zaorsky, Penn State Cancer Institute; James B. Yu, Yale University; Sean M McBride, Memorial Sloan Kettering Cancer Center; William C. Jackson, University of Michigan; Brandon A. Mahal, Dana-Farber Cancer Institute; Ronald Chen, University of Kansas; Ananya Choudhury, University of Manchester and The Christie NHS Foundation Trust; Ann Henry, Leeds Teaching Hospitals, NHS Trust and University of Leeds; Leeds; Isabel Syndikus, Clatterbridge Cancer Centre, NHS Foundation Trust; Timur Mitin, Knight Cancer Institute, Oregon Health and Science University; Alison Tree, Institute of Cancer Research, London; Amar U. Kishan, University of California, Los Angeles.


 February 04, 2026
February 04, 2026 









