May 10, 2016 — Longer time spent by film readers interpreting screening mammograms did not result in a reduced rate of breast cancer detection, according to a study appearing in the May 10 issue of JAMA.
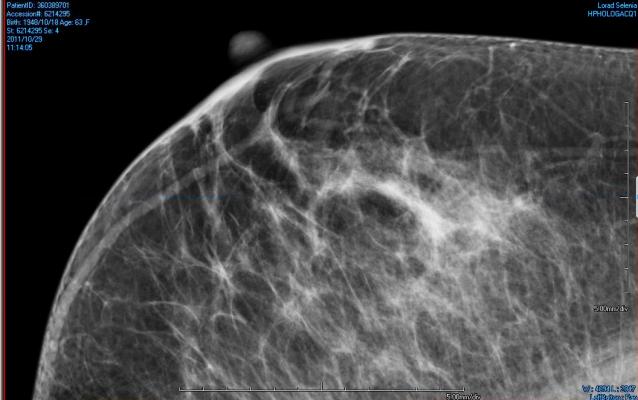
Interpreting screening mammograms is a difficult and repetitive visual search task, for which characteristics of cancer are disguised among background breast parenchyma (tissue), resulting in false-positive recalls and missed cancers. In similar visual search tasks, a vigilance decrement (decreasing detection rates with time on task) has been observed in a large number of psychological laboratory experiments, including assembly line inspection tasks and airport baggage screening. In the United Kingdom (U.K.), two film readers independently evaluate each mammogram for signs of cancer.
Sian Taylor-Phillips, Ph.D., of the University of Warwick, Coventry, U.K., and colleagues investigated whether a vigilance decrement to detect cancer in breast screening practice exists and whether changing the order in which two experts examined a batch of mammograms could increase the cancer detection rate, through readers' experiencing peak vigilance at differing points within the reading batch.
The study was conducted at 46 specialized breast screening centers from the National Health Service (NHS) Breast Screening Program in England for one year. Three hundred sixty readers participated, all fully qualified to report mammograms in the NHS breast screening program. The two readers examined each batch of digital mammograms in the same order in the control group and in the opposite order to one another in the intervention group.
Among 1,194,147 women who had screening mammograms (596,642 in the intervention group; 597,505 in the control group), the images were interpreted in 37,688 batches (median batch size, 35), with each reader interpreting a median of 176 batches. After completion of all subsequent diagnostic tests, a total of 10,484 cases (0.88 percent) of breast cancer were detected. There was no significant difference in cancer detection rate with 5,272 cancers (0.88 percent) detected in the intervention group versus 5,212 cancers (0.87 percent) detected in the control group (recall rate, 4.14 percent versus 4.17 percent; rate of reader disagreements, 3.43 percent versus 3.48 percent).
“The intervention did not influence cancer detection rate, recall rate or rate of disagreement between readers. There was no pattern of decreasing cancer detection rate with time on task as predicted by previous research on vigilance decrements as a psychological phenomenon,” the authors wrote.
For more information: www.jama.jamanetwork.com


 February 18, 2026
February 18, 2026 









