September 25, 2017 — Long-term results of a phase III clinical trial indicate survival rates for patients receiving chemoradiation for unresectable, locally advanced non-small cell lung cancer (NSCLC) may be more than twice as high as previous estimates. At five years following treatment with a standard dose of 60 Gray (Gy) radiation delivered in 30 fractions, the overall survival rate was 32 percent, setting a new benchmark of survival for patients with inoperable stage III NSCLC. The trial, RTOG 0617, also confirms that a standard dose of radiation therapy is preferable to a higher dose and that cetuximab offers no additional survival benefit for these patients. Findings were presented at the 59th Annual Meeting of the American Society for Radiation Oncology (ASTRO), Sept. 24-27 in San Diego.
Lung cancer claims the most cancer-specific deaths of any tumor type, both in the United States and worldwide. The American Cancer Society, using data from the National Cancer Institute, estimates five-year survival rates of 5 to 14 percent for patients who present with stage III NSCLC. RTOG 0617 was a phase III randomized trial that compared a standard radiation therapy dose of 60 Gy in 30 fractions with a higher dose of 74 Gy in 37 fractions for patients receiving concurrent chemotherapy with or without cetuximab for inoperable stage III lung cancer.
“Based on the two-year results reported in 2015, RTOG 0617 has already changed practice and established the standard radiation dose for patients receiving chemoradiation for stage III NSCLC,” said Jeffrey D. Bradley, M.D., FASTRO, the principal investigator of the RTOG 0617 trial and a professor of radiation oncology and director of the S.L. King Center for Proton Therapy at the Washington University School of Medicine in St. Louis.
“When RTOG 0617 was initially reported, the results were surprising to most oncologists because the standard dose of 60 Gy was superior to the higher dose of 74 Gy in this setting. There have been numerous secondary analyses investigating the reasons for this result, and the data point toward greater radiation exposure to the heart in the high-dose arm being the main problem,” he added.
“The current report establishes an overall five-year survival standard for patients receiving standard- dose chemoradiation for stage III NSCLC that is substantially higher than previously estimated. This report also confirms that using a higher radiation dose is not beneficial and can lead to detrimental outcomes including lower survival rates and increase side effects,” Bradley concluded.
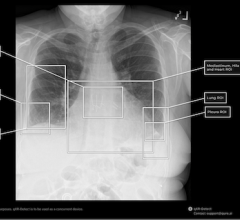
Patients enrolled in RTOG 0617 were randomized to one of two chemoradiation dose groups. Standard-dose treatment consisted of 60 Gy total radiation dose, and high-dose patients received 74 Gy total dose. Radiation was delivered in 2 Gy daily fractions through either intensity-modulated radiation therapy (IMRT) or three-dimensional conformal radiation therapy (3-D CRT). All patients received concurrent weekly chemotherapy with paclitaxel and carboplatin. Patients also were randomized to receive either cetuximab or a placebo.
Across the 185 institutions in the United States and Canada that participated in RTOG 0617, a total of 544 patients with unresectable stage III NSCLC were accrued and 496 were eligible for analysis. The median patient age was 64 years (interquartile range [IQR] 57-70 years). Most patients were male (59 percent) and white (41 percent).The median follow-up for surviving patients was 5.1 years (IQR 4.6 – 6 years).
Survival rates at five years following chemoradiation were higher for patients in the standard-dose treatment arm than for those in the high-dose arm. Median overall survival (OS) following standard-dose treatment was 28.7 months (95 percent CI 24 - 38.4 months), compared with 20.3 months (95 percent CI 18-24 months) for the high-dose cohort (hazard ratio [HR] 1.35, p = 0.004). Five-year OS rates were 32.1 percent and 23 percent for the standard-dose and high-dose arms, respectively (p = 0.004).
Progression-free survival (PFS) rates at five years were 18.3 percent and 13 percent for the standard-dose and high-dose arms, respectively (p = 0.055). Survival rates were estimated using the Kaplan-Meier method and compared using the log-rank test and Cox proportional hazard models.
On multivariate analysis, differences in OS were driven by radiation dose (favoring the standard-dose regimen; p = 0.03), planning target volume (p = 0.022), the accrual volume of the treating institution (p = 0.017), presence of esophagitis/dysphagia (p = 0.008) and V5 heart dose/volume (p = 0.005).
Patterns of tumor recurrence, either in the same location or region as the initial tumor or further away, also favored the standard-dose regimen, although differences between the treatment arms did not reach statistical significance. Failure rates for the standard-dose and high-dose arms, respectively, were as follows: local failure in 38.2 percent versus 45.7 percent (p = 0.068); regional failure in 35.7 percent versus 38.4 percent (p = 0.5); and distant failure in 52.3 percent versus 57.6 percent (p = 0.3). Failure rates were estimated using the cumulative incidence method and evaluated through Fine-Gray models.
Treatment-related side effects were more pronounced with the high-dose regimen. There were three treatment-related deaths in the standard-dose arm, compared with nine in the high-dose arm. Rates of treatment-related grade 3 or higher toxicity for the standard-dose and high-dose arms, respectively, were as follows: dysphagia in 3.2 percent versus 12.1 percent (p < 0.0001); esophagitis in 5 percent versus 17.4 percent (p < 0.0001); and severe pulmonary events in 20.6 percent versus 19.3 percent (p > 0.05).
Cetuximab (delivered as a 400-milligram dose on day one, then 250-milligram doses weekly thereafter) did not confer a benefit for overall survival at five years. Median OS for patients who received cetuximab was 24 months (95% CI 20.4 - 30 months), compared with 24 months (95% CI 20.5 - 28.8 months) for those who did not (HR 1.0, p = 0.048). Moreover, there was no benefit of cetuximab for patients with epidermal growth factor receptor (EGFR) H-scores above 200, counter to earlier findings from the trial.
For more information: www.astro.org
Related Content
Clinical Trials and Cutting-Edge Radiation Oncology Research to Be Featured at ASTRO 2017


 March 05, 2026
March 05, 2026