December 19, 2019 — Hoag hopes to turn the tables on lung cancer by becoming one of select hospitals in the nation, and the first in Southern California, to adopt the Ion robot-assisted bronchoscopy, a technology that drastically improves accuracy and precision of lung cancer biopsy, while also providing an improved patient experience.
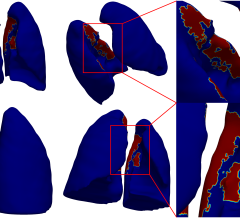
The Ion robotic-assisted bronchoscopy is the newest technology available for lung cancer diagnosis and staging, and now at Hoag thanks to philanthropy. “The current approaches to lung cancer diagnosis have some limitations that the new Ion technology can better address, such as the ability to reach peripheral lung nodules. Nearly 70 percent of lung nodules are detected in the outside lung periphery. This new technology provides greater stability to guide a catheter to these outer nodules, paired with superior navigation. I can view my entire pathway to the nodule as I guide the catheter to it,” said Daryl Pearlstein, M.D., program director for lung cancer at Hoag Family Cancer Institute and a board-certified, subspecialty-trained thoracic surgeon.
During an Ion bronchoscopy, a camera leads the catheter to the nodule, remaining steady and adjusting with the patient’s breath. And because it uses robotic technology, rather than a human, to hold in place, the new technology allows the guiding catheter to remain stable and more still.
In addition to improving access to nodules through stability and navigation, the adoption of this new technology also means an improved experience for patients. “If we could not reach the detected nodule, patients would have to come back for further imaging and biopsy,” continued Dr. Pearlstein. “Other approaches to obtaining a biopsy could also result in a collapsed lung. Utilizing Ion, we enter a patient’s lung in a minimally-invasive fashion, through their mouth into their bronchial tubes.”
Pearlstein also predicts that the Ion will play a role in treating lung cancer, paving the way for a day when many of the estimated 800 lung cancer patients who come to Hoag each year receive diagnosis, staging and treatment all in one office visit.
“Once you detect lung cancer, the traditional treatment involves removing the entire lobe,” he said. “This technology allows us to mark the nodule with a florescent dye, so we can more easily remove just the segment of the lung that has cancer. To put it in terms of breast cancer, it’s like the difference between doing a lumpectomy, rather than a mastectomy.”
Lung cancer is the second-most common cancer in the U.S. and among the deadliest. Yet, when detected early, lung cancers can be very treatable.
“In the past, lung cancers were diagnosed at an advance stage, when the prognosis was poor,” Pearlstein said. “Now high-risk individuals are more likely to receive annual CT scans, so more are being successfully treated for lung cancers at earlier stages. Unfortunately, there is still often a two- to three-month delay between when a nodule is noticed on a CT scan and when a diagnosis and determination of a cancer’s stage could be made.”
This new technology promises to reduce that time considerably, improving patients’ prognosis and quality of life.
“Hoag has all the latest treatment modalities for lung cancer: targeted chemotherapy, advanced clinical trials, Cyberknife, robot-assisted surgery. But you can’t treat a tumor until you have a diagnosis and staging,” Pearlstein said. “This technology will allow us to compress the time between detecting a nodule and getting treated. This is such a benefit to the patients.”
While that day is still off in the future, Pearlstein noted that the investment the philanthropic community has made in Hoag brings patients and their families closer to more effective, efficient lung cancer care. Only one other hospital in California has this technology, and few in the nation have the community support that has allowed Hoag to make these types of advances.
For more information: www.hoag.org


 January 23, 2026
January 23, 2026