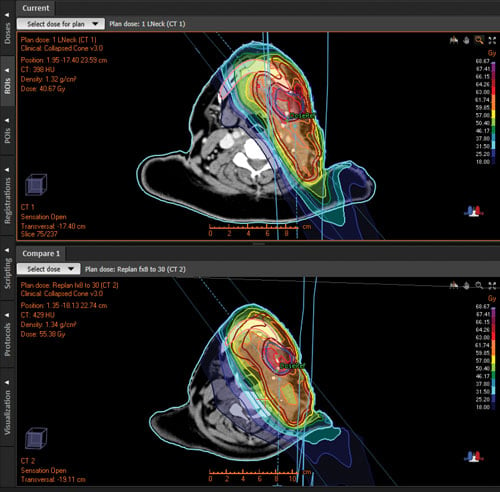
Clinical Example
A patient with left mubmandibular cardinoma, node positive, was treated with adjuvant radiotherapy to the submandibular region and ipsilateral neck following radical surgery. Anatomical changes during treatment resulted in the mandible dose being over the accepted threshold. PTV does cover was also compromised due to changes in CTV. Replanning brought Dmax to mandible to winin accepted limits. PTV and CTV were also turned to the optimal range.
The Radiation Oncology Department at Auckland City Hospital, New Zealand, has made great strides in boosting efficiency over the last few years, while taking quality of treatment to new levels. It’s a shift in which technology has played a significant role. Today, the department is a pioneer of adaptive therapy. It also boasts one of largest VMAT programs in Australasia and operates a completely paperless workflow.
The department serves around one-third of the New Zealand population — 1.5 million people — over a large geographical area that stretches from 100 km south of Auckland to the northern tip of the country. With 100 staff members and six LINACS, it runs almost 4,000 courses of radiation therapy per year.
Giuseppe Sasso, M.D., the department’s clinical director, says the right treatment planning system is an essential factor in making adaptive therapy work on a large scale.
“Investing in RayStation has given us a far superior planning infrastructure,” Sasso said. “Adaptive therapy demands a high-speed planning system, combined with high-quality imaging. It’s only feasible with a system such as RayStation, which is extremely fast and has excellent tools for the clinician.”
Improving on the Plan
Sasso’s main clinical focus is on head and neck, prostate and breast cancers. His department assesses patients for adaptive therapy as a matter of routine, based on set parameters for volume changes.
“Tumors shrink during radiation therapy,” Sasso said. “Naturally we need to adjust the volumes. But the shrinkage does not always follow the expected geometry, which means there is a risk of the plan missing the clinical target volume. Adaptive therapy ensures you are always on target.”
Sasso stressed that adaptive therapy is not just about preserving the original plan.
“The relationships between GTV, CTV and PTV are constantly changing, so planning is like solving a complex puzzle with many dynamic variables. Replanning can make it possible to achieve a dosimetry that is even better than the original plan, with reduced impact on organs at risk.”
Optimizing the Workflow
Auckland City Hospital’s approach is highly protocolized for consistency. Around 30-40 structures are contoured for every patient, and rescanning is done using a high-quality planning computed tomography (CT). The team puts a great deal of care into keeping the contours as consistent as possible day to day, for example through ensuring patients always have a moderately full bladder and an empty bowel.
“RayStation’s algorithms for adaptive therapy and deformable registration work extremely well with our protocolized workflow,” Sasso said. “When a new plan is proposed, a radiation therapist will assess the new GTV and CTV, and we do most corrections using the 3-D mesh tool. It takes just a few drag-and-drop moves. The algorithm is very accurate, so little modification is needed.”
Depending on the case, replanning with RayStation may take just a matter of minutes. “For prostate patients it’s quite simple,” Sasso stated. “But even complex head and neck cases go fast. Running the whole process within RayStation gives us a warm start. Things are much slower if you have multiple systems and need to transfer data between them.”
Focused Organization
Auckland City Hospital’s Radiation Oncology Department has also made important changes in its organizational structure and focus. The workflow is now based on tumor streams. Teams are smaller, and individual staff have a greater level of specialization, creating clusters of advanced expertise. Overall, this approach has resulted in greater efficiency and consistency.
Training is a key focus, Sasso said. “For our program to be sustainable, everyone in the treatment chain needs to practice at a very high level. Our people are passionate about what they do, and we have built a culture of pride in efficiency and good use of resources. That’s one of the reasons we use RayStation for adaptive planning. Our approach needs to make the best possible use of public funds.”
Paperless System
The move to a paperless system has delivered another major boost to efficiency, Sasso said. “The only paper we have now is the consent form. Doctors often work offsite and a paperless system with remote access, such as RayStation, makes things faster and simpler. Streamlining every interaction is important when you have high volumes. This can enable you to do many more adaptive replannings in a year. One of the strengths of RayStation is that it enables a fast and seamless interaction with the patient journey.”
Case study supplied by RaySearch.


 February 11, 2026
February 11, 2026 









