
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group.
BLOG: How Advances in Technology Help Patients and Providers
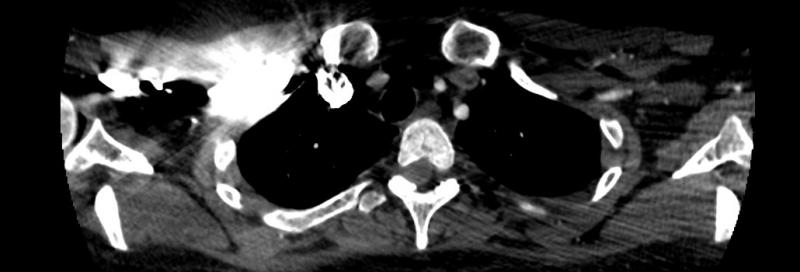
Power injectors can improve efficiency and patient safety, for example, ensuring that contrast agent is not wasted due to the lack of a saline bolus. Image courtesy of Lior Molvin
Patient safety and operational efficiency are behind the development of modern contrast media, selection and utilization strategies — as well as refinements in the injector technologies for these media. Much remains to be done.
New agents for MRI and diagnostic sonography were created to get the most from these imaging modalities, which do not rely on ionizing radiation — gadolinium-based agents for MRI; bubble agents for diagnostic ultrasound. The development some three decades ago of nonionic iodinated contrast agents exemplifies the importance of patient safety as a force underlying the development of modern contrast agents.1, 2
Similarly, low-osmolar nonionic contrast agents for CT may have fewer side effects and less nephrotoxicity than traditional ionic, high-osmolar agents. Intravenous MRI contrast agents are not toxic to the kidney, but the development of NSF (nephrogenic systemic fibrosis) is a continuing concern, say opinion leaders. The clinical significance and reason for gadolinium accumulation in tissue among patients without renal impairment, they say, is not known.
It is known, however, that the nonionic molecules of gadolinium chelates have lower osmolality and viscosity, which makes them more digestible at higher concentrations and allows faster bolus injections.3
Sonographic agents use microbubbles to improve the diagnostic yield,4 while maintaining safety.5
Technological Evolution Picking Up
From now on, however, much of the innovation involving contrast-enhanced studies will likely involve the power injector. And its evolution could be dramatic.
Just as the cell phone has become much more than a phone, contrast injectors are evolving into new — and different —- roles. Injector-oriented technologies, for example, are already available in the management of protocols and the supply chain. These tools could help assess waste, the number of extravasations, technologist performance, site and shift performance, even department budgets.
“Beyond the obvious ability to standardize injections (to achieve) image consistency, there are so many opportunities for injectors to become clinical devices that cannot be lived without,” said Lior Molvin, a CT technologist and protocol manager for the diagnostic CT group at Stanford Health Care in Palo Alto, Calif.
Simple algebraic tools might be built into injectors, Molvin said. Power injectors could help departments with “just-in-time” supply, for example. This would improve efficiency by reducing the need to over stock contrast agents. “The injector would know exactly how much contrast it has injected, so we would know how much we need to order in order to maintain operational efficiency,” he said. The injector might even link to a data base associated with the ordering cycle.
Injectors could also automatically consider the size of the patient — tall or short; skinny, average or obese — saving time that technologists otherwise may spend factoring body habitus into injection strategies and protecting patients from over- and under-dosing. Even more might be accomplished with the integration of smart algorithms that check the circumstances surrounding extravasations, especially as they pertain to CT and MRI.
Greg Freiherr is a contributing editor to ITN. Over the past three decades, he has served as business and technology editor for publications in medical imaging, as well as consulted for vendors, professional organizations, academia, and financial institutions.
Editor’s Note: This is the second blog in a series titled Using Contrast Media. The first blog, Why Power Injectors Are Needed for High-quality Imaging, can be found here. How customer needs factor into product innovation will be the focus of the next blog in this series.
References:
- Pradubpongsa P, Dhana N, Jongjarearnprasert K, et al. Adverse reactions to iodinated contrast media: prevalence, risk factors and outcome-the results of a 3-year period. Asian Pac J Allergy Immunol. 2013;31(4):299-306. https://www.ncbi.nlm.nih.gov/pubmed/24383973
- McClennan BL. Ionic and nonionic iodinated contrast media: Evolution and strategies for use. AJR Am J Roentgenol. 1990;155(2):225-233.
- Hunt CH, Hartman RP, Hesley GK. Frequency and severity of adverse effects of iodinated and gadolinium contrast materials: Retrospective review of 456,930 doses. AJR Am J Roentgenol. 2009;193:1124-1127. https://www.ncbi.nlm.nih.gov/pubmed/19770337
- Ignee A, Atkinson, NSS, et.al. Ultrasound contrast agents. Endosc Ultrasound. 2016 Nov-Dec; 5(6): 355–362. http://www.eusjournal.com/article.asp?issn=2303-9027;year=2016;volume=5;issue=6;spage=355;epage=362;aulast=Ignee
- Ultrasound Societies Urge FDA to Remove Black Box Warning on Contrast Agents https://www.itnonline.com/content/ultrasound-societies-urge-fda-remove-black-box-warning-contrast-agents


 February 04, 2026
February 04, 2026 









