March 2, 2015 — Disparities in the level of awareness and knowledge of breast density exist among U.S. women, according to the results of a Mayo Clinic study published in the Journal of Clinical Oncology.
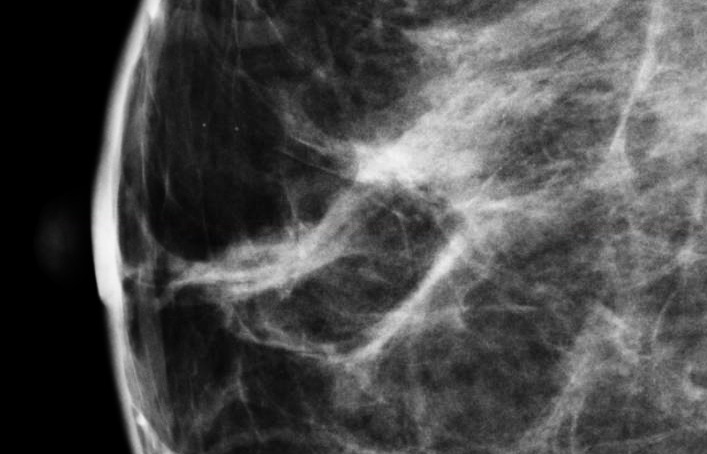
Breast density is the term used to describe the variation in dense tissue on a mammogram image. Fatty breast tissue appears more radiologically translucent than dense (fibroglandular) breast tissue. Regions of a breast that comprise fatty tissue will appear darker on a mammogram, while regions that comprise dense tissue appear whiter.
Increased breast density has been shown to mask cancers on the mammogram as well as to be associated with future risk of breast cancer. Recent legislation in several states mandates that women be given information about breast density in order to guide decisions about breast cancer screening.
Researchers conducted a national cross-sectional survey of 2,311 women ages 40 to 74 in English and Spanish. The survey response rate was 65 percent. Overall, more than half of women who responded (58 percent) had heard of breast density, 49 percent were aware that breast density affects breast cancer detection and 53 percent knew that breast density is associated with cancer risk.
When researchers examined the survey results for race and ethnicity, they found increased breast density awareness among white, non-Hispanic women relative to minority women. Increased awareness was also associated with women with higher household incomes, women with higher education, women who had received a diagnostic evaluation after a mammogram and women who received postmenopausal hormone therapy.
"The results of our study support the need for continued efforts to improve awareness of breast density and its implications on screening among women who are eligible for screening mammograms," says the study's lead author, Deborah Rhodes, M.D., a consultant in preventive medicine at Mayo Clinic.
Rhodes and colleagues also found that respondents from Connecticut were more likely than residents of other states to be aware of the potential masking effect of breast density on mammographic detection of cancer and were more likely to have discussed breast density with a healthcare provider. Connecticut was the first state to pass breast density legislation in 2009. To date, legislation mandating disclosure of breast density information has been passed in 21 states.
For more information: www.mayoclinic.org


 February 23, 2026
February 23, 2026 









