GE's whole-body 7T MR system at the University of California, San Francisco QB3 site demonstrates its magnetic power as a paper clip floats in the air.
New whole-body imaging techniques are widening the scope of vision into the details of biological function. By using whole-body PET/CT, scientists are tracking immune system cellular activity in real time. Simultaneously, investigators are optimistic about advances in whole-body MRI, where MR improves the ability to identify metastatic spread and MR angiography has proven instrumental in detecting carotid and peripheral vascular disease.
PET/CT Captures Cells in Real Time
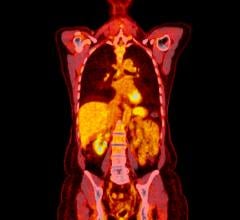
Clinicians are discovering the tremendous advantages gained from whole body imaging on the positron-emission tomography computed tomography (PET/CT) hybrid systems. New techniques in whole-body PET/CT have widened the aperture for evaluating cellular information, allowing clinicians to watch immune system cells’ activity. Clinicians are using images to visualize how immune cells identify and respond to tumors or infection, and track how the tumor reacts throughout the different phases of the immune response process. According to Owen N. Witte, M.D., professor of Microbiology, Immunology and Molecular Genetics, UCLA, and an investigator of the Howard Hughes Medical Institute, whole-body PET/CT can render a broader view of the immune system and is a significant improvement over snapshot views captured through tumor biopsies or blood assays.
Highlighting tracers in organs is another advantage of whole-body PET/CT. One of Siemens’ works-in-progress that it will present at the Radiological Society of North America’s (RSNA) 92nd Scientific Assembly and Annual Meeting 2006 is the development of a computer-aided detection (CAD) program that can detect internal organs such as the kidney in PET/CT images and evaluate the efficacy of discounting normal physiological uptake of [(18)F]fluorodeoxyglucose (FDG) by these organs. In the study, researchers imaged 66 patients with lung cancer, liver cancer, breast cancer or lymphoma using PET/CT. A computer program that automatically detected internal organs such as the kidney, bladder, heart and liver was based on a learning framework in which the user trains a discriminative classifier that recognizes a local region containing the organ of interest. In kidney detection, if the detected region corresponds to a hot spot (SUV >2.5) in PET, the hot spot is interpreted as relating to physiological uptake by the kidney. Then a segmentation method is applied to delineate the boundary of the kidney hot spot, and statistics on kidney hot-spot SUV values are collected.
Based on their results, researchers determined that computer systems can be trained to detect internal organs that have high physiological FDG uptake, such as the kidney, hence enabling hot spots that correspond to physiological uptake to be accurately interpreted and discounted. This leaves only hot spots that correspond to pathological uptake, such as in tumors, in PET images.
Whole-Body MR Broadens its Reach
While MR is prevalently used to image the brain, spine, the soft tissue of joints and inside of bones, researchers are discovering new applications in other areas of the body such as the prostate and the abdomen.
“With the introduction of whole-body MRI, which offers better sensitivity and higher specificity in detecting bone metastasis, we’re moving into the next phase of MRI diagnostic capabilities,” said Joseph Constance of Kalorama Information, a healthcare research firm that recently released a report on the growth of MRI.
The next phase of MRI lays in identifying metastasis in the abdomen. The greatest challenge for abdominal MR exams is that one in 10 are rendered inconclusive due to motion artifacts or inadequate resolution. To remedy this problem, GE Healthcare has integrated its MR systems Signa HD 1.5T and Signa HD 3.0T with a new MRI software called LAVA (liver acquisition with volume acceleration). LAVA combines contrast-enhanced, multiphasic imaging with fat suppression for MR liver imaging. The MR system can scan the entire liver of a large patient in a single breath-hold, which is particularly helpful with patients who have difficulty holding their breath, and LAVA reportedly achieves 25 percent more resolution with 25 percent more coverage compared to other standard MR devices.
MRS for Prostate
As prostate cancer has become one of the leading cancers in the U.S., affecting one in six men, prostate spectroscopy and imaging have become increasingly important in detecting and staging prostate cancer.
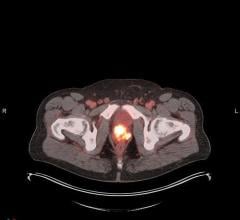
The procedure involves scanning the entire pelvis and entails integrating prostate spectroscopy and imaging into a clinical MRI staging exam for prostate cancer. One of the first noninvasive diagnostic systems that works with MRI to detect, localize and stage tumors in the prostate is GE Healthcare’s PROSE. In the presence of prostate cancer, there is decreased citrate and choline increases due to a rise in proliferation membrane changes and increased cell density. Once the MR captures an image of the prostate, clinicians can evaluate the levels of choline and creatine to pinpoint the location of the tumor, as well as stage and determine the aggressiveness of the cancer.
“At UCSF we add a spectroscopy (3-D MRSI) sequence to all patients receiving a high-resolution MRI staging exam for prostate cancer, and have scanned over 3,200 patients to date,” said John Kurhanewicz, Ph.D., University of California, San Francisco. “Because the ability to detect and determine the spatial extent of cancer using MRI alone is hampered due to therapy-induced morphologic changes, we believe that MRSI will have its greatest impact on assessing the effectiveness of prostate cancer therapy.”
New MR Techniques Track Metastases
One technique that is gaining interest in oncology is diffusion-weighted whole-body imaging with background body signal suppression (DWIBS), which produces PET-like images similar to FDG-PET imaging. This sequence has been developed to detect lymph nodes and to differentiate normal and hyperplastic from metastatic lymph nodes.
“We are watching some of the applications of body imaging with three tesla, and whole-body diffusion looks quite promising at giving you a tool to rapidly look for cancer metastases,” said Chris Farr, vice president of Sg2, a healthcare research and consulting firm.
In a study led by Tsuyoshi Komori, M.D., Ph.D., Osaka Medical College, department of Radiology, investigators compared DWIBS and FDG-PET/CT to determine which modality is more useful for evaluation of malignant tumors. Researchers evaluated the apparent diffusion coefficient (ADC) value (_10-3 mm2/sec) and the standardized uptake value (SUV) in the cancer lesions for quantitative evaluation of DWIBS and FDG-PET, respectively. The findings indicated that DWIBS was more feasible than FDG-PET/CT in the detection of cancers, however, DWIBS might still be challenged in differentiating between the benign and malignant lesions using the ADC values.
An increasingly popular whole-body MR sequence applied to metastasis screening is T2-weighted short tau inversion recovery (T2 W STIR) MRI. The combination of noncontrasted T1-weighted-spinecho sequences and fat suppressed short tau inversion recovery-(STIR)-imaging is known to be very accurate for detecting bone marrow lesions including metastases.
Since robust segmentation of the spinal cord is a reliable reference object in automatic vertebrae segmentation, an important works-in-progress that Siemens will present at RSNA 2006 is a study to develop a fully automatic algorithm for spinal cord detection in T2 W STIR images. Xiang Zhou, Ph.D., Siemens Medical Solutions, and his team have found that 3-D-polynomial modeling provides a fully automatic rapid and reliable estimate of centerline position and segmentation of the spinal cord. The new application will be used for spinal cord examination, metastasis screening, multimodal registration, curved MPR visualization and automatic vertebrae segmentation.
Metabolic MRI
Leveraging the power of whole-body 7T MR research to rapidly develop products from bench to bedside, the University of California, San Francisco (UCSF) and GE Healthcare are collaborating in the development of new technology that tracks real-time changes in tissue metabolism.
“Although MR images are widely used in a clinical setting, the information they provide is often limited, resulting in diseases such as cancer being detected only late in their cycle – when treatments are costly or ineffective,” said Sarah Nelson, Ph.D., UCSF professor of Radiology and director of the Surbek Laboratory of Advanced Imaging at QB3. “Improved characterization of the disease is critical in efforts to influence the chances of survival and make more treatment options available. The high-field MR scanners at QB3 will significantly improve sensitivity and specificity, allowing us to more effectively target therapy and provide noninvasive biomarkers of response to new therapies.”
The goal of the collaboration between UCSF and GE is to facilitate the current paradigm shift taking place in molecular medicine – to predict the onset of disease at the earliest possible stage, before symptoms appear.
With the ability of high-field MR to image nuclei in the body such as sodium, phosphorus, oxygen and carbon, researchers anticipate that these nuclei may provide disease-specific molecular and functional information unobtainable on conventional MRIs, and thus detect disease in a way that was previously unachievable.
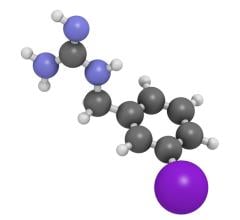
In a study aimed at measuring a biochemical fingerprint of tissue for earlier diagnosis, improved staging and influence treatment in prostate cancer, researchers at UCSF are using a metabolic MR imaging technique with a Carbon 13 agent to light up pyruvate. The evolution and progression of prostate cancer is known to correspond changes in the metabolic fluxes through citric acid cycle, glycolysis and fatty acid synthesis. As researchers analyze the real-time metabolism of 13C1-pyruvate, elevated levels of lactate and intravascular pyruvate also light up in the MR image to reveal how the cancer has spread. While the agent is currently only used in clinical trials for the prostate, it could have applications in other organs in the future.
Whole-Body MRA in Growth Mode
Whole-body MR angiography (MRA) has become a viable alternative to conventional digital-subtraction-angiography (DSA) for atherosclerosis, a systemic disease affecting multiple areas of the body. Early detection of atherosclerotic vascular disease is crucial for diagnosing and evaluating systemic atherosclerotic disease. Due to the systemic nature of atherosclerotic disease, clinicians must apply techniques to assess the entire arterial vascular system. Furthermore, common manifestations of prior ischemic disease can be found in the heart and the brain.
In a study by Tuebingen, Eberhard-Karls University, Germany, radiologists introduced an innovative MRA protocol using a dedicated whole-body MR-scanner, a 1.5T Magnetom Avanto by Siemens, with 32 receiving-channel technology. Whole-body MR scanners with surface coil technology enable whole-body MRA examinations to provide information of the patient’s complete arterial vasculature. The new coil technology produced whole-body MRA examinations without patient repositioning, while providing high SNR in short measuring times. The images revealed systemic atherosclerotic disease covering the arterial vasculature from intracranial arteries to distal runoff vessels. Further evaluation of organs predisposed to atherosclerotic disease revealed cerebral or cardiac disease.
The potential for comprehensive staging of vascular involvement of systemic atherosclerotic disease prompted Siemens to release the Magnetom Trio, a 3T whole-body MRI system with Tim (total imaging matrix technology). Tim technology enables flexible coil combinations for high-resolution imaging of large anatomical areas without the need to change coils. MRA studies can be acquired from the top of the head to the lung in 20 seconds or a whole torso MRA in 20 seconds or less. This 3T system supports parallel imaging for peripheral angiography. Its 36-element Peripheral Angio Matrix coil performs high-speed, whole-leg, high-resolution MRA.
Large Bore Whole-Body CT
Where whole-body CT imaging is making strides is with specific tasks such as imaging for radiation therapy and for interventional or bariatric procedures.
Responding to the increased need for coverage, resolution and power, GE introduced the LightSpeed RT16 for radiation therapy simulation and planning, and the LightSpeed Xtra, a 16-slice CT scanner designed for radiology versatility, including imaging for interventional and bariatric procedures. The LightSpeed RT16 is built with an extra large 80 cm gantry opening for better patient positioning and for clinicians to image the patient’s entire anatomy. The scanner’s 4DCT software for radiation oncology fuses 4-D imaging and planning for radiotherapy. AdvantageSIMT MD also integrates 4-D data into the planning process and provides multimodality/multiphase simulation for treatment like IMRT and IGRT.
To address the problem of obesity in the U.S., the LightSpeed Xtra is a new wide-bore CT system designed to overcome the challenges of imaging larger patients to capture quality images.
Seeing Through a Whole New Light
Possibly one of the most innovative perspectives of whole-body imaging is seen through fluorescent scanning. For nearly a decade, scientists have used green fluorescent proteins as beacons to other proteins or gene promoters to illuminate numerous biological processes. Now, one researcher is using visible light to illuminate a process known as optical fluorescence molecular tomography (FMT) and produce 3-D anatomical renderings based on CT data. Developed by a team led by Vasilis Ntziachristos, HMS assistant professor of Radiology at Massachusetts General Hospital, the technique uses visible light to illuminate fluorescent proteins and to quantitatively reconstruct their location from inside tissues, in order for researchers to track cells that express fluorescent proteins within the entire body. The procedure is aimed at assisting clinicians in monitoring the growth of tumors and the delivery of viral genes. Today, the study shows that you can actually quantify the number of green fluorescent proteins in living animals. The researchers hope that soon it will light up proteins in people.




 February 03, 2026
February 03, 2026