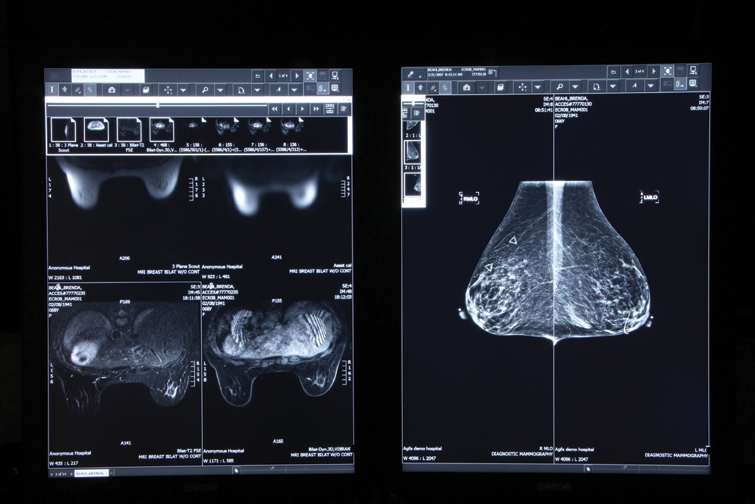
Dense breast tissues make mammograms (right) difficult to read, which may require complementary testing, such as MRI (left). Efforts by state legislatures mandating that physicians inform patients of the challenges of dense breast imaging raise both opportunity and risk for readiologists.
For many years mammographers have been saddled with low reimbursements. Recognizing this, women’s health advocates lobbied successfully last decade for higher rates for mammograms produced with digital equipment.
This may be the only exception to the “rule of less” that has been applied to imaging reimbursements since the federal Deficit Reduction Act (DRA) took effect in 2007. Cutbacks in reimbursement have at the very least slowed the growth of medical imaging procedures and led to a decline in the purchase of new imaging equipment, just as the increased reimbursement for digital mammography led to a boom in the purchase of full-field digital systems that today dominate the landscape of women’s health.
While the federal government has been content to influence the practice of medicine through financial dictates, individual state governments lately have taken a more direct approach. Five states now mandate physicians to inform women with dense breasts that mammography may be of limited value for them. Connecticut, Virginia, Texas, California and New York require physicians to advise patients that complementary imaging studies, such as ultrasound or MRI, may be needed if dense fibroglandular tissues are likely to obscure the mammographic signs of cancer.
This legislation offers opportunity for radiologists, who might do what the RSNA at its last annual meeting advised members to do: “Be the voice of radiology for your patients.” They might educate and inform patients about the significance of breast density, as they are doing at the Elizabeth Wende Breast Clinic in Rochester, N.Y. They might also provide complementary testing. It is logical to expect that they do so. But stepping into this breach carries risk. (Editor’s Note: For more information, see “Legislating Women’s Health: A Chance for Radiologists to Step In” by Greg Freiherr at http://bit.ly/YOG3Mh.)
Third-party payers in the first states to adopt such mandated education have typically reimbursed for the ultrasound procedures that may follow, although its not required by law. And while ultrasound coverage may be provided, it is seldom there for the MRI exams that might be indicated for women with dense breasts at high risk of developing cancer. When reimbursement is not available, the laws do not address who should shoulder the costs.
And there are logistical challenges, as well. Few mammography practices have the capacity to perform ultrasound immediately following the determination that a patient has dense breasts. Even fewer can accommodate an MRI exam the same day. Patients found to have dense breasts and prescribed a complementary exam, therefore, may have to return for another appointment or travel to another facility, neither of which may be easy, particularly if they have traveled a long way for their mammogram already.
Then there are fundamental problems with ultrasound and MRI. Their high sensitivity and lack of specificity lead inevitably to more biopsies and a preponderance of negative findings for procedures that otherwise would not have been performed, as illustrated by early experiences in the first state to enact such legislation, Connecticut.[1]
Consequently, legislative efforts of this type amount to little more than unfunded mandates that impose costs on insurance companies, practitioners and patients. While they may provide an opportunity for radiologists to become more involved with patients, radiologists must be careful in how they respond to this opportunity, as these mandates may expose them to risks that can endanger the very relationships that they foster.
At least when the federal government seeks to influence medical practice, it foots the bill…albeit at a cut rate.
Greg Freiherr has reported on developments in radiology since 1983. He runs the consulting service, The Freiherr Group. Read more of his views on his blog at www.itnonline.com.
1. Hooley RJ, Greenberg KL, Stackhouse RM, Geisel JL, Butler RS, Philpotts LE. “Screening U.S. in patients with mammographically dense breasts: initial experience with Connecticut Public Act 09-41.” Radiology. 2012;265:59-69. Abstract: www.medscape.com/medline/abstract/22723501.


 February 18, 2026
February 18, 2026 









