2006 - 2007 SNM President Martin P. Sandler, M.D., Vanderbilt University Medical Center, Department of Radiology and Radiological Sciences
“I think quantification is the next big breakthrough in imaging technology,” said the 2006 – 2007 SNM President Martin P. Sandler, M.D., of Vanderbilt University Medical Center, Department of Radiology and Radiological Sciences, in an interview with Imaging Technology News (ITN) on the future of nuclear medicine.
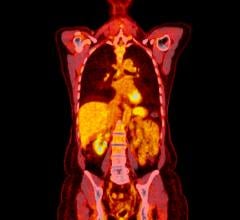
The Society of Nuclear Medicine (SNM) has embarked on a mission to improve healthcare by advancing molecular imaging and therapy, and the SNM 2007 conference program will feature an increased presence of related research. ITN talked to Dr. Sandler about how nuclear medicine will drive personalized medicine in the future.
ITN: How is molecular imaging using imaging technology such as PET, SPECT, MRI and others to develop personalized medicine?
Martin P. Sandler, M.D. (MS): It is the understanding of how cellular function and biological processes of the cell work from the receptor through the cell membrane all the way to the inner functions of the cell. By looking at different receptor sites and different activities of the cell one can develop specific imaging and therapeutic interventions that will be tailored for individuals based on the ability of the receptors to respond to specific probes as well as certain therapeutic interventions.
ITN: How has molecular imaging and nuclear medicine research led to improvements in the diagnosis and treatment of cancer, heart disease and brain disorders?
MS: It has the potential to affect a large variety of diseases, including cardiac disease, and various cancers. We have already seen it with monoclonal antibodies and there is the possibility of that certain brain disorders have the potential to be responsive, as well. It covers a host of different diseases.
ITN: Can you describe what the new program InfoSNM involves and what the objective is?
MS: We have developed a number of live, interactive lifelong learning programs and people can access the educational component and with that is a continuing medical education component that goes along with these. These are live, interactive programs. There is also training of clinicians and technologists with hybrid imaging, which is a key part of the molecular imaging process or where by you have a congruence of different technologies giving different synergistic kinds of information.
ITN: Exactly which hybrids are you referring to?
MS: These hybrids include PET/CT, SPECT/CT and also work being done on PET/MRI.
Simon Cherry, who gave the Henry Wagner lecture at last year’s SNM, showed that scientists have overcome the technical challenges of integrating PET and MRI imaging. There are models now that are being worked on now.
PET/MRI has the advantage s there is of less radiation and MR gives different kinds of information, such as MR spectroscopy’s the ability to overlap MR spectroscopy on a tumor and look at its therapeutic response. All of the different roles of MR versus CT can now be combined potentially with PET, as can CT.
ITN: What are some of the advancements you anticipate will develop in Nuclear Medicine over the next five years?
MS: Besides the translational development of new products and nanoparticle technology, I think that the biggest advancement will be bringing quantitative measurements to the bedside. If you look at cardiac imaging today, we are looking at relative blood flow. We steal blood from parts of the heart that have narrowing of blood vessels and look at compare it to other parts of the heart with normal blood flow. With pharmacological exercises we improve blood flow, we increase blood flow and we look at relative diminishment in blood flow. I think that we are soon going to have technologies, which have high enough contrast count rates and resolution such that we will have the same sensitivity for gamma camera imaging as we do with PET. This will allow us to quantitate absolute blood flow and the ml/min diminish for 100 grams of tissue. I think quantification is the next big breakthrough in imaging technology.


 February 03, 2026
February 03, 2026