The design of Leksell Gamma Knife PERFEXION expands the treatment reach, offering a wider range of treatable anatomical structure.
Fighting cancer is serious business. Every day in hospitals and cancer clinics worldwide, radiation oncologists, neurosurgeons and physicists combat the disease in its myriad forms with the help of medicine’s most sophisticated tools and technologies. As radiation therapy continues to evolve, the latest cancer treatments are not only becoming more precise, but also more widely available.
As little as 10 years ago, for example, intensity-modulated radiation therapy (IMRT) was only offered at a few university hospitals; today, virtually every radiation center has IMRT.
“I began using IMRT in 2000 and since that time the technology has grown and become more refined and more user-friendly,” said Michael Greenberg, M.D., radiation oncologist and medical director at the Dale and Frances Hughes Cancer Center in East Stoudsberg, PA. “Now we use image-guided radiation therapy (IGRT), which is basically IMRT with the ability to track — through the use of implantable fiducial markers and image guidance — the motion and position of a tumor.”
Dr. Greenberg and his colleagues use Varian’s SmartBeam IMRT, on-board imager (OBI) IGRT, cone-beam CT (CBCT) and respiratory gating (RPM) tools to treat their patients.
“The nice thing is that it is seamless. We go from the management and scheduling system to the treatment planning computers, to the accelerators and to the simulators — there are no breaks in networking. We find the ability to have one integral component talk with the other is very efficient,” Dr. Greenberg said.
To better manage respiratory motion when delivering dose, Dr. Greenberg uses Dynamic Adaptive Radiation Therapy (DART), which allows for on-the-fly dosimetry adjustments with the position each day. “Right now, we make the slight shifts and then give the treatment, but DART will enable us to actually see the slight variations that the shift causes in the dose every day,“ Dr. Greenberg explained.
Another tool for patient positioning is BrainLAB’s ExacTrac X-ray 6D IGRT. The system automatically corrects patient set-up errors and tracks patient movement throughout the procedure. The system’s treatment indications include the prostate, lung, liver and spine.
One of the newest institutions to install ExacTrac 6D is Central Arkansas Radiation Therapy Institute (CARTI), a seven-facility practice located in Little Rock, AR, which adopted the technology in order to improve treatment of malignant and nonmalignant tumors.
“The implementation of the BrainLAB ExacTrac X-Ray 6D system makes the advanced treatment technology available for our patients,” said CARTI Radiation Oncologist Ann Maners, M.D. “Thanks to the high level of accuracy built into BrainLAB technology, we now have the ability to administer more accurate treatments, which should result in fewer complications.”
Whole brain radiation therapy alternative
For patients with metastatic brain tumors, radiosurgery is often the treatment of choice. One of the most popular radiosurgical techniques involves the Gamma Knife from Elekta. The device’s latest version is the Gamma Knife Perfexion, and the first site in the U.S. to install and use the system is Washington Hospital Healthcare System’s Fremont Hospital in California.
Fremont first used the Perfexion — an alternative to traditional whole brain radiation therapy — in June 2007 on a female patient who had three metastatic lung cancer deposits in the brain.
“This patient had lung cancer and a huge advantage of the one-day Perfexion treatment was that she had no break in her chemotherapy,” said David Larson, M.D., PhD, FACR, radiation oncologist and co-director of Washington Hospital Healthcare Gamma Knife program. When chemotherapy is suspended in patients with metastatic disease, he explained, the systemic cancer continues growing. Standard radiation, on the other hand, which takes several weeks, can’t be administered in conjunction with chemotherapy.
The outpatient Perfexion procedure can be performed on patients with a target volume of up to 3 cm in size in either the head or neck. A maximum of 192 narrow beams of radiation enter the patient’s head from a wide variety of angles. When all 192 beams are used the dose distribution produced is spherical and as small as a few millimeters in diameter.
“For targets that are nonspherical, the dose distribution can be customized to different sized targets by moving the focus point into different positions,” Dr. Larson explained. “Multiple focal points within the target are treated with thousands of tiny beams, all in one or two hours.”
Taking local control
“One of the challenges of benign or malignant tumor treatment is local control,” said Dr. Larson. “The beauty of radiosurgery is that it delivers an extremely high dose of radiation to the target, and the dose drops off extremely rapidly just adjacent to the target.”
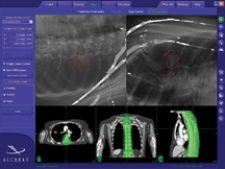
Lung cancer patients, in particular, may benefit from radiosurgery’s precise target control. Accuray’s Xsight Lung Tracking System — designed for use with the CyberKnife Robotic Radiosurgery System — noninvasively treats lung tumors through its ability to track their movement directly without fiducial markers. It delivers highly specialized soft tissue tracking by using the actual image intensity of the lung tumor to target the beam, which eliminates, in some cases, the need for implanted fiducial markers.
“The CyberKnife System with Xsight Lung Tracking allows us to break down the barriers to lung cancer treatment. We are now able to give new hope to patients — such as the elderly and those considered medically or surgically inoperable — who previously would have had no other option,” said James Schwade, M.D., executive director of the CyberKnife Centers of Miami and Palm Beach.
An additional tool in Accuray’s cancer treatment arsenal is the Monte Carlo dose calculation methodology, which received FDA 510(k) clearance in September. The Monte Carlo dose calculation is designed to enable clinicians to more precisely determine, in a matter of minutes, the intensity of radiation to be delivered in areas where tissue densities vary. This is particularly beneficial when treating lung cancer, since healthy tissue surrounding tumors is made up of air cavities, which are less dense than the solid tumors.
“Incorporating Monte Carlo dose calculation capabilities into the CyberKnife System will enable clinicians to quickly and precisely plan treatment and accurately determine the resulting radiation delivered to tumors,” said Charlie Ma, PhD, director of Radiation Physics at Fox Chase Cancer Center in Philadelphia.
Protons vs. photons
Proton therapy is a highly advanced form of cancer treatment that is potentially more effective than the X-rays (photons) conventionally used in radiation therapy, as protons target tumors more precisely and deliver more cancer-killing energy to the treatment area, while sparing nearby healthy tissue.
“With conventional radiation from linear accelerators, the X-rays that are generated keep traveling until they hit something. There is some interaction with tissue before the radiation hits the target, and some dose is delivered beyond the target,” William F. Hartsell, M.D., co-Medical Director of Radiation Oncology at Advocate Good Samaritan Cancer Center, Downers Grove, IL, president of Radiation Oncology Consultants Limited (ROCL) explained. “Protons are different. Because they are charged particles, they go a certain distance, stop and then give off their energy. No dose is given beyond the target and the dose to normal tissue around the target volume is limited.”
Proton therapy is currently only available in five specialized treatment facilities in the U.S., and ground has been broken for two more. But there have been changes, says Dr. Hartsell, that are making it easier for physicians in community hospitals to bring the technology to their patients. For one, more vendors today are building proton machines and reimbursement is now available.
ROCL, a single-specialty group of 12 radiation oncologists in Chicago, IL, and its surrounding areas, in conjunction with ProCure Treatment Centers Inc., is working to bring the technology to a suburban community hospital, making it the first center in the Illinois to offer proton therapy. Pending regulatory approvals, patient treatment is expected to begin in 2010 at Central DuPage Hospital, Winfield, IL.
Although proton therapy is slowly becoming more available and the technology is becoming more practical due to improvements in imaging and dose calculations, one drawback still remains. Protons must be accelerated to sufficiently high energies, currently only achieved with very large and very expensive cyclotrons or synchrotrons.
Thomas Mackie, a professor at the University of Wisconsin and co-founder of TomoTherapy, is working on a proton-therapy design based on a much smaller device known as a “dielectric wall accelerator” (DWA) that would fit in a conventional radiation treatment room. The DWA prototype is being built at Lawrence Livermore National Laboratory, Livermore, CA, and according to the American Institute of Physics Web site, can accelerate protons to up to 100 million electron volts in just one meter. A two-meter DWA could potentially supply protons of sufficiently high energy to treat all tumors, including those buried deep in the body. In addition, a DWA-based proton therapy system could also vary both proton energy and proton-beam intensity, two variables that cannot both be adjusted at the same time in existing proton-treatment facilities. This capability could lead to “intensity-modulated proton therapy” (IMPT), the proton version of the X-ray-based IMRT.
The increasing number of treatment facilities that offer proton therapy, along with the DWA system scheduled to be in clinical trials in about five years, have opened the door to yet another type of radiation therapy becoming a more accessible option for cancer treatment.



 January 30, 2026
January 30, 2026