In a comparison of patients with Stage-1 non-small cell lung cancer (NSCLC) during the period 1999-2008, those in the last four years of that period who received radiation therapy had a median survival rate of 21 months, which was markedly better than the 16-month rate among similar patients in the first four years. These study results were presented by lead author Nirav S. Kapadia, M.D., chief resident, department of radiation oncology, University of Michigan Medical School, during the 2012 Chicago Multidisciplinary Symposium in Thoracic Oncology.
The event was sponsored by the American Society of Clinical Oncology (ASCO), American Society for Radiation Oncology (ASTRO), International Association for the Study of Lung Cancer (IASLC) and the University of Chicago, and held in Chicago in September. The study1 was based on an analysis of the SEER-17 (Surveillance Epidemiology and End Results) National Cancer Institute database, which encompasses about 25 percent of the United States population.
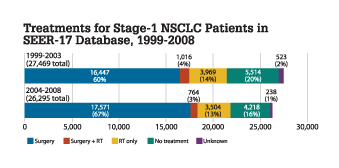
The study compared outcomes for 27,469 patients in the database from 1999-2003 with 26,195 patients from 2004-2008. Patients were treated with surgery, radiation, a combination of both, or received no treatment. As shown in the graph comparing treatments for both groups, there was an increase in surgery, from 60 to 67 percent, and a slight decrease in radiation therapy, from 14 to 13 percent. There was a drop in the number of patients who did not receive any type of treatment, from 20 to 16 percent. However, Kapadia feels this number remains too high.
“At least 16 percent of patients are still not getting the care that they need, care that could save their lives,” he said. “We must identify the barriers to treatment so that every patient has hope for a cancer cure.”
The study did find that overall survival for all patients, regardless of the type of treatment, improved about 27 percent in the latter four years as compared to the earlier period. The median survival rate increased from 44 to 56 months. Also, for patients who received only radiation, survival improved by five months, or 31 percent.
Radiation Therapy Improvements
Radiation therapy traditionally is given to patients who are deemed too sick to undergo surgery, which remains the primary and preferred modality for treating this type of cancer, Kapadia said. But he noted the recent advances made in radiation therapy, particularly with stereotactic body radiation therapy (SBRT), which enable increased doses to be given to the tumor while avoiding damage to surrounding healthy tissue.
Kapadia also noted that radiation therapy offers some advantages to surgery, because it is noninvasive, can be done as an outpatient procedure and the track record of survival for patients who are too sick for surgery is very good. He added that there are several ongoing trials, mostly outside the United States, examining radiation versus surgery, and they could have interesting results.
“I would say the advances in radiation have been pretty dramatic in the last decade or so
and will continue to be, in my humble opinion,” Kapadia said. itn
Reference:
1 NS Kapadia, WO Quarshie, FD Vigneau, AG Schwartz, FP Kong. “Patterns of Practice and Outcomes for Stage-1 Non-Small Cell Lung Cancer (NSCLC): Analysis of SEER-17 Data 1999-2008.” Presentation at 2012 Chicago Multidisciplinary Symposium in Thoracic Oncology.


 January 30, 2026
January 30, 2026 









