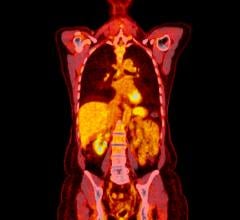
The Precedence SPECT/CT system from Philips Medical Systems
In the past, nuclear medicine had been coined “unclear medicine” by cynics because of its inability to target exactly where disease is located in the body. The uncertainty was not in the ability of functional imaging to determine a problem, but in localization. The introduction of hybrid imaging is working to change all of that, however, and SPECT/CT technology is providing clinicians with the tools to characterize metabolic activity in the body, and where it is taking place. As many as 60 percent of SPECT/CT procedures are done in cardiology, but orthopedics, oncology and infection imaging are emerging as areas that can benefit from SPECT/CT as well. With ever-increasing multislice CT technology expanding applications of SPECT/CT, it is doing its part to make nuclear medicine a clear choice for disease diagnosis.
Finding a Spot in the Marketplace
SPECT/CT’s sister technology, PET/CT, pioneered hybrid imaging in nuclear medicine, but the later arrival does not translate into substandard diagnostic capabilities. SPECT/CT and PET/CT have different areas of influence and their own areas that assist in diagnostic decision-making. One major difference between the two is the contrast agents used. PET/CT uses positron-emitting isotopes like fluorine-18 FDG or C-11, while SPECT/CT predominately uses technetium-99 and iodine-131, which are single photon isotopes. Another difference is PET/CT’s better spatial resolution due to higher count rate and coincidence detection. However, SPECT/CT’s inferior spatial resolution is not inhibiting its adoption, which experts believe has a bright future.
“We believe that SPECT/CT will continue to have an increased adoption rate over the next several years,” said John Liebig, senior product manager for SPECT/CT, Philips Medical Systems. “We don’t expect it to be as rapid as what we realized in PET/CT, but we definitely see the market moving towards SPECT/CT over the long term.”
Partha Ghosh, M.D., clinical marketing manager, Molecular Imaging, Siemens Medical Solutions, also believes that SPECT/CT is the device of the future. For this reason, Siemens is focusing hard on research and development of SPECT/CT, which has paid off as the adoption rate is growing very fast. He believes that the interest in the technology across the world stems from its convenience. Another reason adoption rates may see rapid increase is cost. From an equipment and pharmaceutical standpoint, SPECT/CT is the less expensive option.
“In terms of comparison between PET and SPECT procedures, PET procedures generally demand a premium because the drug is more expensive, and it is much more difficult to distribute,” said Liebig. “[PET pharmaceuticals] typically have a shorter half-life and require a cyclotron to produce the drug. [PET] also is a more expensive piece of equipment.”
Although the technology has its benefits, there are several factors hindering its complete adoption. Among these barriers are limited use and technical issues, such as ensuring absolute registration.
The first problem is the limited knowledge on techniques and clinical applications for the new advanced SPECT/CT systems. Currently, there are very few published articles describing the value of the technology. As more and more systems are being used, evaluations in scientific publications will drive the value of the technology, increasing physicians’ interest and confidence level in using CT more effectively with SPECT.
Second, there are still technical difficulties involved. “One of the key challenges is ensuring the absolute registration between the emission data and the CT data,” said Liebig. “We are always working on new ways to improve that registration and make sure that it is quantifiable and reproducible.”
Given the existing molding of the equipment, Dr. Ghosh is “very sure that people are going to appreciate what the new technology brings to them, and they will be fast followers.”
Emerging Applications
While SPECT/CT is being used heavily for cardiology applications, such as calcium scoring and computed tomography angiography (CTA), SPECT/CT will be increasingly utilized in the three emerging areas of orthopedics and sports-related medicine, oncology and infection imaging.
Physicians are seeing a marked increase in orthopedic SPECT/CT procedures. Liebig stated that Stephen C. Scharf, M.D., chief of Nuclear Medicine at Lenox Hill Hospital in New York, NY, who works with Philips, has seen a significant increase in the procedures performed at his site because he is able to show the functional imaging attributes in combination with high-resolution CT. SPECT/CT can identify disease or conditions that even MR can’t, and orthopedics can be viewed as an up-and-coming category in SPECT imaging.
In the area of oncology, SPECT/CT can serve patients who do not have FDG-friendly cancer. While the isotope does a great job at localizing disease in PET/CT, not all cancers can be detected by FDG. Thyroid, parathyroid, neuroendocrine and prostate gland tumors are examples.
“There are roughly 225,000 new cases of prostate cancer each year, and there is no PET derivative that effectively works those patients through the system,” said Liebig. “In the area of SPECT and SPECT/CT, there is a drug called Prosticent, which can effectively localize in the area of disease in the prostate, and we are finding the potential to better characterize prostate cancer with SPECT/CT in oncology.”
Using SPECT/CT for infection imaging may be a solution to the dilemma of a patient presenting at the hospital and going through a series of procedures before arriving at a diagnosis. It is believed that with white blood cell tagging, gallium and other agents available in the SPECT sphere, SPECT/CT could be the go-to scan. If this expectation is realized, the patient could avoid the additional procedures, making SPECT/CT a very efficient mechanism for infection patients.
Dr. Ghosh emphasized that SPECT/CT is being used effectively for neurological applications as well. “SPECT/CT has many advantages in terms of better attenuation correction of the brain,” he said. “Also, sometimes a contrast CT also gives an idea of the degree, if there is any other disease like a tumor or infarct, particularly in the situation where the patient has Alzheimer’s, but it is actually caused by vascular problems like multiple early infarct.”
SPECT/CT Systems Continue to Evolve
Philips Medical Systems and Siemens Medical Solutions are two of the leading manufacturers of multislice SPECT/CT systems. Philips offers the Precedence 6-, 16-, and 64-slice SPECT/CT systems and Siemens offers the 2- and 6-slice Symbia TruePoint SPECT/CT.
Philips debuted the 64-slice Precedence SPECT/CT at the American Society of Nuclear Cardiology (ASNC) in Montreal, Canada in September 2006. The 64-slice Precedence SPECT/CT is the first system to offer 64-slice CT capabilities, and has the benefit of being a full 64-slice diagnostic CT system, a full diagnostic SPECT system and a combination hybrid.
“The Precedence 64 is the only device that can do myocardial perfusion imaging with attenuation correction, calcium scoring and coronary CTA all on the same device in one episode of care,” said Liebig.
The Symbia TruePoint SPECT/CT from Siemens is also capable of performing multislice CT exams, SPECT and SPECT/CT scans. Dr. Ghosh noted that Siemens currently offers the 2- and 6-slice options because they find them optimum for certain applications, such as cardiac and bone disease. In the future, Siemens will work on developing software.
“What we are trying to do is get much more into software,” said Dr. Ghosh. “We are trying to improve on the image processing, make it faster. We are trying to make SPECT acquisition faster so that we can do more patients in a shorter span of time.”
The marriage of SPECT and CT is doing its part to rid nuclear medicine of its “unclear medicine” moniker. With constant upgrades in multislice CT technology, physicians are afforded the opportunity to increase the technology’s applications and clearly see metabolic activity in the body and where it is located.



 February 03, 2026
February 03, 2026