July 7, 2014 — The ability to generate patient specific mammographic dose using volumetric breast density data from 2-D mammography and 3-D tomosynthesis was among the research presented at the 12th International Workshop on Breast Imaging (IWDM 2014), June 29-July 2, 2014. According to Volpara Solutions, while radiation dose in mammography is low the breast is radio-sensitive, which makes minimizing dose in mammography while maximizing image quality a critical part of any quality assurance program.
The patient-specific dose research is one of multiple abstracts that highlight the use of quantitative breast imaging software tools to provide Enterprise-wide breast care imaging and informatics, including volumetric density, patient-specific dose and applied pressure.
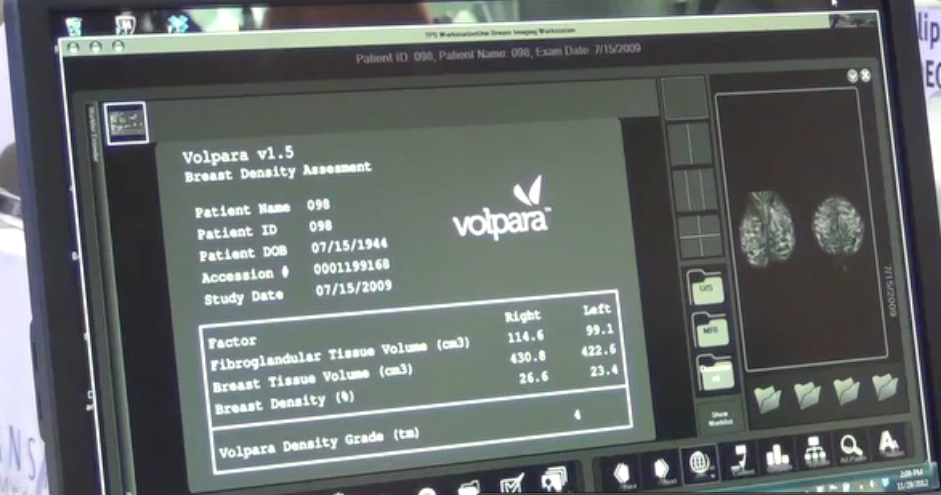
In the study, “Patient Specific Dose Calculation using Volumetric Breast Density for Mammography and Tomosynthesis,” researchers demonstrated how to calculate a patient-specific mean glandular dose (MGD), which personalizes dose to the individual woman using her volumetric breast density, rather than assuming a certain breast density, or one that is estimated solely from compressed breast thickness. Patient-specific MGD values were generated using Volpara volumetric breast density measurement software to estimate the glandularity, or percentage of the breast that contains glandular tissue, of each breast from the mammogram, and the MGD calculation method presented by Dance et al. Researchers compared the values calculated using VolparaDensity with those reported by the manufacturer for a database of 403 2-D mammograms.
While agreement is good for dense breasts, results demonstrated that the MGD is underestimated in fatty breasts. Results for 91 2-D projection images and 3-D tomosynthesis acquisitions in “combo” mode were also compared. In general, the MGDs are approximately equal; however, when split into density categories, it becomes apparent that breasts exhibited significantly different doses, with tomosynthesis MGDs being higher than mammogram MGDs for fattier cases.
“The results of this study reinforce that volumetric breast density supports the ability to calculate personalized MGD estimates using the patient specific glandularity. Manufacturer reported MGD estimates appeared to underestimate dose in the case of fatty, or low density, breasts in comparison to our calculations, but gave good agreement in the case of dense breasts,” said Ralph Highnam, Ph.D., CEO of Volpara Solutions and a co-author. “When comparing MGD in combined tomosynthesis/mammography examinations, at lower breast density the mammographic dose is lower than in tomosynthesis, but at higher density the dose is approximately equal, or even less. This is a factor that should probably be considered when evaluating which patients should get tomosynthesis versus mammography.”
With growing emphasis on dose in medical imaging as a result of the Image Wisely initiative, it is reasonable to expect dose monitoring to expand to include mammography. The Size Specific Dose Estimation (SSDE) for computed tomography (CT) was created by an AAPM Task Group in response to the fact that reported dose is not patient-specific but the dose to a standard phantom. Likewise, most mammography units today routinely under- or over-estimate dose because they provide a dose, which does not include the patient’s specific volumetric breast density in the estimation. Additionally, since the algorithms used vary, the estimations are not easily compared.
VolparaDose is vendor-neutral and uses patient-specific quantitative data to generate a more accurate assessment of the MGD per image. Research shows that it is possible to improve the accuracy and personalization of radiation dose estimation, which can allow you to identify safety issues, and keep your patients better informed.
“The breast is among the organs most sensitive to radiation, and it is therefore essential to keep X-ray mean glandular dose as low as possible, while achieving as diagnostically useful an image as possible, for fear of inducing cancers during mammography and/or tomosynthesis screening,” added Highnam. “The introduction of breast tomosynthesis and of shorter screening intervals for high-risk women potentially increase patients’ exposure to radiation dose, which has renewed interest in the accurate MGD calculation, tracking and accountability on an individual patient basis.”
Cleared by the U.S. Food and Drug Administration (FDA), HealthCanada, the TGA and CE-marked, VolparaDensity is used by radiologists to objectively assess density from both digital mammography and tomosynthesis images and help evaluate who might benefit from additional screening. Highly correlated to breast magnetic resonance (MR) assessments, VolparaDensity is a reliable tool which automatically generates an objective, automatic measurement of volumetric breast density and a FDA cleared BI-RADS breast density category. More than 3 million women have had their volumetric breast density analyzed using VolparaDensity, which is part of a suite of quantitative breast imaging tools built on the Volpara algorithm which enables volumetric measurements of density, patient specific dose, breast compression and other factors designed to help maintain accuracy and consistent quality in breast screening.
For more information: volparasolutions.com


 February 18, 2026
February 18, 2026 









