Maintaining the financial health of your radiology practice is key to helping you address the physical health of your patients. After all, if your group practice is ailing financially, no one stands to gain any long-term benefits. Ensuring the ongoing viability of your practice is not always simple, but it need not be burdensome. Like a plan or a scan related to physical health, if you establish a regimen, continually track vital indicators and receive regular checkups, then the financial health of your practice is within reach.
All healthy medical practices have these factors in common: effective income management, effective expense management, strategic planning and involved partners.
Effective income management includes assessing the market in which you practice, assessing the structure in which you practice, including relationships with medical centers, payers and other medical groups, and managing your accounts receivable (AR).
Effective expense management includes managing the direct costs of the services you provide, managing the indirect or overhead costs of your practice, identifying and eliminating costs that do not contribute to your service or practice structure and reducing your financial risks. Moreover, be actively involved with your partners in the business side of your practice. At minimum, provide regular oversight and strategic direction.
Market Factors
One area of practice health often overlooked by hospital-based physicians is market positioning. Evaluate these factors periodically: venues, volumes and control (VVC):
1. Where are the key venues where you provide services to the patients?
2. Where is the patient population or volumes coming from (payers, employers, medical groups, etc.)?
3. Who controls where services are provided?
Also evaluate your group’s position relative to the market and develop strategic plans to maintain or capture more VVC.
Another market indicator is the strength and satisfaction of your referral and customer base – typically physicians and patients. Don’t overlook hospital administrators, payers and vendors. Routinely assess satisfaction levels of all these constituents through formal and informal marketing efforts and respond to concerns as another method to maintain a healthy market position.
Control Over Contracts
Radiologists can exert more control over their professional service and payer contractual arrangements. For example, if a hospital or facility insists that your radiologists do more for less, review the service contract. Is there room for renegotiation? If not, are there other opportunities for you to provide input? Payer contracting and monitoring is also essential. Negotiating intelligently with carriers — and assessing their performance — requires accurate, relevant data. Develop contract matrices and monthly payer summaries. These summaries help isolate problems when they start, help track and address compliance issues and reestablish benchmarks to measure results.
Making AR Work Harder
AR is nonproductive, since funds are tied up and do not produce additional income. Therefore, over time, its value erodes. Radiologists are particularly vulnerable to AR problems. They are dependent upon third-party payment, while providing critical clinical services without questioning a patient’s ability to pay. In order to realize payment for services, radiologists are increasingly turning to new business partnerships to optimize collections and improve the health of their practice.
Every radiologist should question the current AR process. Ask, “How can we do this better?” Small problems quickly become large ones if corrective measures aren’t taken. A classic example is a claims denial, in which a particular payer rejects a regularly submitted CPT code. Left unchecked, expect a buildup in AR. Eventually, someone will have to review every claim and pull documents, prepare an appeal and work at resolution. Avoid wasting time and energy correcting a problem that could have been prevented if caught early.
“With dwindling reimbursements, exams must be coded properly,” says Sheri Hockett, M.D., president of Imaging Consultants of Garland, TX. “Radiology practices cannot afford to simply write off denied claims as if it were an accepted component of ‘business as usual.’”
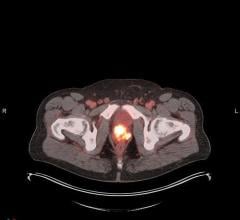
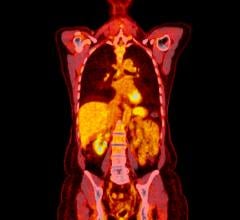
Dr. Hockett added, “Our claims that were most vulnerable to denial were the most complex procedures and higher RVUs — such as CT, MRI and ultrasound. It’s this level of complexity that creates a critical need for expert coders to handle claims.”
A similar drain of resources arises when two sets of claims are submitted in close succession, resulting in overpayment. Be sure to track a few basic revenue metrics: gross revenue last month vs. this month, gross revenue this month vs. this month last year, charges and credits, average AR days and percent of AR over 120 days. Also, question any change in the normal pattern of income, as a group and individually. The problem could be as simple as a change in practice patterns, the impact of a delay in reimbursement from a specific payer or as disastrous as a breakdown in the compensation formula.
Review the Processing Environment
Consider your processing environment as it relates to AR and information management. For example, electronic claims processing saves money, improves cash flow (with up to 99 percent accuracy, thanks to electronic editing), enhances staff productivity and supports compliance. Radiologists who use this tool and others such as paper-claim mining, Web-based reporting of practice results and database profiling of practice billing patterns, will make more effective practice decisions.
“Expert coding, proper reporting and harmonious data are all crucial elements in running a healthy radiology practice,” said Dr. Hockett. “Additionally, it’s useful to know payer requirements for claim submissions — the preferred format for submission, when and how to use modifiers, etc. Meeting these specifications will help ensure the claim can be processed accurately the first time.”
“We chose outsourcing as a cost-effective solution that incorporates advanced reporting capabilities and electronic billing that can serve the complexities of our business,” said Dr. Hockett. “The additional revenue generated via correctly coded claims alone makes it a worthwhile investment. We have increased our collections by approximately 16 percent since we started outsourcing. Supporting an in-house billing staff would require constant training for changes in payer requirements, coding procedures and government regulations, which proves expensive and time intensive.”
Identify Other Financial Indicators
Initially, a thorough review of expenses should be performed and compared to industry standards. Many practices overlook the opportunity to reduce or at least control what would be considered nonbeneficial costs. Factors such as productivity standards (for physician and nonphysician staff) should be examined to determine if appropriate staffing levels are being achieved and whether benchmarks could be established to measure performance improvement.
Also, conduct profitability assessments by site, location, modality and by
procedure level. As hospitals, payers and patients continue to demand more services at more locations, such profitability information becomes invaluable for healthy decision-making.
The Impact of Compliance
Consider compliance in the overall health of your practice. A thorough compliance program includes:
1 A Practice Assessment: analysis of claims data with regard to all applicable governmental and state billing requirements for third-party payers.
2. A Compliance Plan: standards of conduct identified for employees in a plan that is realistic, practice-specific and integrates with the group’s management structure. A documented and implemented plan helps protect your group in the event of an audit.
3. Physician In-Service Training: communicates (a) why standards of conduct must be developed, (b) the potential impact of noncompliance and (c) the specific aspects of behavior that must be modified.
4. Ongoing Monitoring: a critical element identified by the Office of the Inspector General; reflects periodically extracting and analyzing a meaningful sample of physician charges.
5. Enforcement: without it, no significant or permanent change can occur.
6. Billing Policies and Procedures: a physician’s primary tool for education must include input from physicians at all sites to ensure all potential billing situations are addressed.
A strong, growing and profitable practice needs to balance many elements. Whether you outsource or internally manage AR and other business management functions, a comprehensive practice review by an external consultant can confirm what’s on target and identify potential improvements. When well executed, a review offers new perspectives and serves as an invaluable, in-depth evaluation to help prioritize short- and long-term challenges and opportunities for maintaining a financially healthy practice.
Feature | November 09, 2006 | Jeff Wescott
The formula for a healthy medical practice includes effective income management, expense management, strategic planning and involved partners.
© Copyright Wainscot Media. All Rights Reserved.
Subscribe Now


 February 03, 2026
February 03, 2026