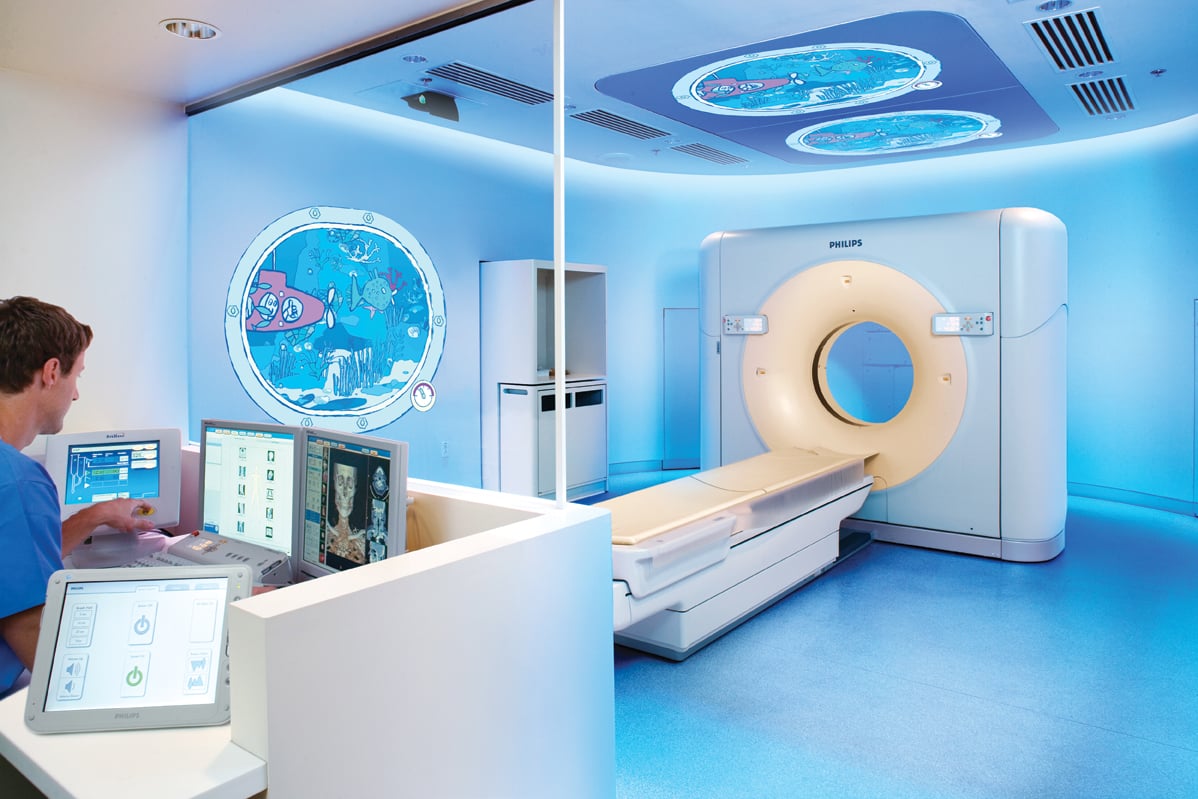
The Philips Healthcare Ambient Experience helps create a relaxing atmosphere for pediatric patients.
Imaging children has challenges that relate to the size, maturity and anxiety of the patient. In addition, we have become increasingly aware of the risks associated with radiation exposure, an issue that is of paramount importance to young patients. Through the efforts of professional organizations, industry and the Image Gently campaign, launched in 2008 by The Alliance for Radiation Safety in Pediatric Imaging, tremendous advancements have been made in technology and its use to help meet these challenges.
Imaging often relies on the cooperation of the patient to obtain a diagnostic result. For this reason, appropriate patient preparation is pivotal, particularly in the pediatric population. Age-appropriate information regarding the various aspects of a procedure can go a long way in obtaining both patient satisfaction and diagnostic results. The pediatric patient and caregivers alike will find the experience less stressful — and patients will be more likely to hold still — resulting in the radiologist and referring healthcare providers obtaining useful diagnostic information. Child life specialists are tremendously helpful in preparing a child for an imaging procedure, and a child-friendly environment helps create a less frightening atmosphere. Faster scan times also help to improve diagnostic results by decreasing motion artifact.
Dose Reduction
With recent technological improvements, the utilization of computed tomography (CT) increased dramatically in all patients. Of note is the increased use of CT in the pediatric population for the question of appendicitis. The literature has shown that ultrasound is an excellent alternative to CT for this clinical question, with the benefits of no ionizing radiation and lower cost. Analysis of long-term sequela has demonstrated that the most cost-effective strategy is to use ultrasound to determine if a child has appendicitis, and then resort to CT in equivocal cases. This algorithm, used at many pediatric institutions, incorporates a strategy that is effective in reducing dose to patients: using modalities that do not require ionizing radiation in place of those that do. Although this concept is simple, the practice of using modalities without ionizing radiation, or not imaging at all, is the best way to decrease radiation exposure to patients.
CT is an outstanding modality and often is the modality of choice for a given clinical situation. The radiologist must work together with the medical physicist and technologist to develop protocols that provide diagnostic image quality while following the as low as reasonably achievable (ALARA) principle. There are many practical articles and resources on the Image Gently website to assist in this process. The imaging team can tailor examinations for the clinical question; for example, more noise may be tolerated in a CT performed to evaluate the osseous configuration of the chest in a child with pectus excavatum in which calculation of the Haller index is the main clinical question. CT parameters such as the tube current (mAs) and peak kilovoltage (kVp) should be adjusted according to the patient size and weight. Lower mAs result in less dose but more noise. In comparison to the linear association of mAs to dose, kVp is exponentially related to dose, but again, lower kVp results in lower dose but more noise or quantum mottle. Shielding may be helpful in reducing dose to radiosensitive organs, but the appropriate use of these devices, such as bismuth breast shields, must be considered in light of additional tools that may be built into the CT scanner.
Most CT scanners have built in methods of dose reduction. These include automated tube current modulation, automated tube potential selection and iterative reconstructions.
Tube Current Modulation (Automatic Exposure Control)
Because of the anatomical and tissue differences in various regions of the body, there are variations in the amount of radiation absorbed at different anatomic regions. As the X-ray tube rotates around the patient, there is a difference in the thickness of the patient; for example, anteroposteriorly versus laterally. Angular tube current modulation varies the tube current to result in a more consistent number of photons reaching the detector. The mAs value is selected by the operator, and the variations are determined by the initial scout radiograph obtained in the CT scanner. Longitudinal tube current modulation modifies the current in the z-axis to even the photons reaching the detector, which would otherwise vary due to the anatomic differences encountered, such as in the pelvis versus the lungs. Both angular and z-axis modulation may occur concurrently. This technique can reduce dose by reduction of the number of photons used in regions with less absorption of radiation.
Tube Voltage
As previously noted, decreased tube voltage results in a lower dose. Assessment of the individual patient can be performed to determine the optimal kVp, but this method is time-consuming for the imaging team. There is one set of CT scanners with an automated process that factors in the patient’s body habitus, region being scanned and the type of scan. The appropriate mAs is determined by the scout radiograph. Lower kVp is strategically used in CT angiographic studies.
Iterative Reconstruction
Filtered back projection (FBP) was the standard mathematical model for CT reconstruction. This method is particularly good with low noise. With the demand for lower dose studies and increasing tolerance for noise, the use of iterative reconstructions has become more common. Improvements in hardware have made it feasible to perform the computations necessary in a timely manner. The basic methodology of iterative reconstructions is a repetitive reformation that attempts to meet a standard. These reconstructions can be performed either in the data derived directly from the CT or after the initial reconstruction, which is less time-consuming. Currently, no manufacturer has an algorithm that relies on reconstructions performed exclusively with the data directly from the CT. There are some that combine iterative reconstructions with FBP. The images obtained with this iterative technology can have a smooth appearance; using a combination of both reconstruction techniques can both decrease this appearance and the time required to view images. By allowing for acquisition of images that would have unacceptable levels of noise using the standard FBP, iterative reconstructions provide another technique to reduce dose.
Resources Available
Although there are challenges in imaging the pediatric patient, there are a variety of resources available to assist in this endeavor, including the website www.imagegently.org, and technological advances in CT scanning such as automatic exposure control, automated tube potential selection and iterative reconstructions.
Sabah Servaes, M.D., is the director of CT, director of the radiology residency and director of the pediatric radiology fellowship at the Children’s Hospital of Philadelphia, as well as a member of the CT Committee of the Society for Pediatric Radiology.
Sjirk J. Westra, M.D., is associate radiologist/associate professor at Massachusetts General Hospital for Children. His main research and community service interest has been to look at outcomes of pediatric imaging through involvement in risk/benefit studies and development of appropriateness criteria.




 February 13, 2026
February 13, 2026 









