Sept. 10, 2012 — High mammographic breast density, which is a marker of increased risk of developing breast cancer, does not seem to increase the risk of death among breast cancer patients, according to a study led by Gretchen L. Gierach, Ph.D., of the National Cancer Institute (NCI), part of the National Institutes of Health. The research was conducted in collaboration with investigators from the NCI-sponsored Breast Cancer Surveillance Consortium (BCSC).
In the study of more than 9,000 women with a confirmed diagnosis of breast cancer, high mammographic density was not associated with the risk of death from breast cancer or death from all causes combined. The study appeared Aug. 20, 2012, in the Journal of the National Cancer Institute.
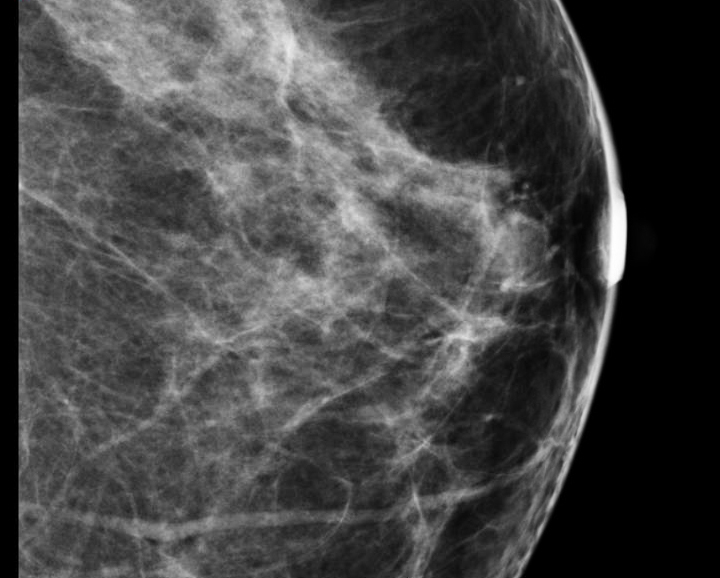
Mammographic breast density reflects the tissue composition of the breast as seen on a mammogram. High mammographic density appears as extensive white areas on an X-ray. Glandular and connective tissue, together known as fibroglandular tissue, block the passage of X-rays to a greater extent than fatty tissue. Breasts with a greater proportion of fibroglandular tissue are said, therefore, to be mammographically denser. For most women, mammographic breast density decreases as they get older, reflecting gradual replacement of fibroglandular tissue by fatty tissue during the normal aging process.
Although high mammographic breast density is a well established risk factor for developing breast cancer, it was unclear prior to this study whether breast density is also associated with the risk of death among women diagnosed with breast cancer. To address this question the scientists analyzed data from the BCSC, a population-based registry of breast imaging facilities in the United States. The scientists restricted their analysis to five BCSC registries that consistently collect data on body mass index (BMI). BMI is a poor prognostic factor for breast cancer that is inversely related to breast density and therefore might potentially affect associations between density and breast cancer death.
Patients included in the study were 30 years or older at breast cancer diagnosis, which occurred primarily between January 1996 and December 2005. The patients were followed, on average, for 6.6 years, at which time 1,795 deaths were reported, including 889 from breast cancer and 810 from other causes. To analyze breast density, the scientists used the most widely available measure of breast density currently in clinical use, a score known as the Breast Imaging-Reporting and Data System score, which is given by a radiologist based on visual review of a mammogram. Data on tumor characteristics and other personal and health factors were also analyzed.
The analysis of mammographic density showed that breast cancer patients with high-density breasts did not have a higher risk of death from breast cancer than patients with lower density breasts, after adjusting for other health factors and tumor characteristics. The lack of an association between mammographic breast density and breast cancer death is consistent with findings from an earlier, smaller study that examined this association.
This study also found an increase in risk of breast cancer death associated with lower breast density among specific subgroups, particularly breast cancer patients who are obese. The authors speculate that one possible explanation for the increased risk associated with low breast density among some subgroups is that breasts with a higher percentage of fat may provide a tumor microenvironment that facilitates cancer growth and progression.
"Overall, it was reassuring to find that high mammographic breast density, one of the strongest risk factors for breast cancer, was not related to risk of death from breast cancer or death from any cause among breast cancer patients," said Gierach. "Given that we identified subsets of women with breast cancer for whom low density was associated with poor prognoses, our findings underscore the need for an improved understanding of the biological components that are responsible for breast density."
NCI leads the National Cancer Program and the NIH effort to dramatically reduce the burden of cancer and improve the lives of cancer patients and their families, through research into prevention and cancer biology, the development of new interventions, and the training and mentoring of new researchers. For more information, visit www.cancer.gov.
For more information about NIH and its programs, visit www.nih.gov.
To read a report on the study from the American College of Radiology (ACR), click here.


 February 05, 2026
February 05, 2026 









